The Falls Risk Assessment categorizes an individual's risk of falling into low, moderate, or high categories. It helps identify problem areas (gait, strength, balance) that must be addressed to reduce fall risk.
Falls Risk Assessment
Uncover the essentials of Falls Risk Assessment. Learn what it is, how it works, and its benefits. Plus, get a free PDF download for practical application.
Falls Risk Assessment Template
Commonly asked questions
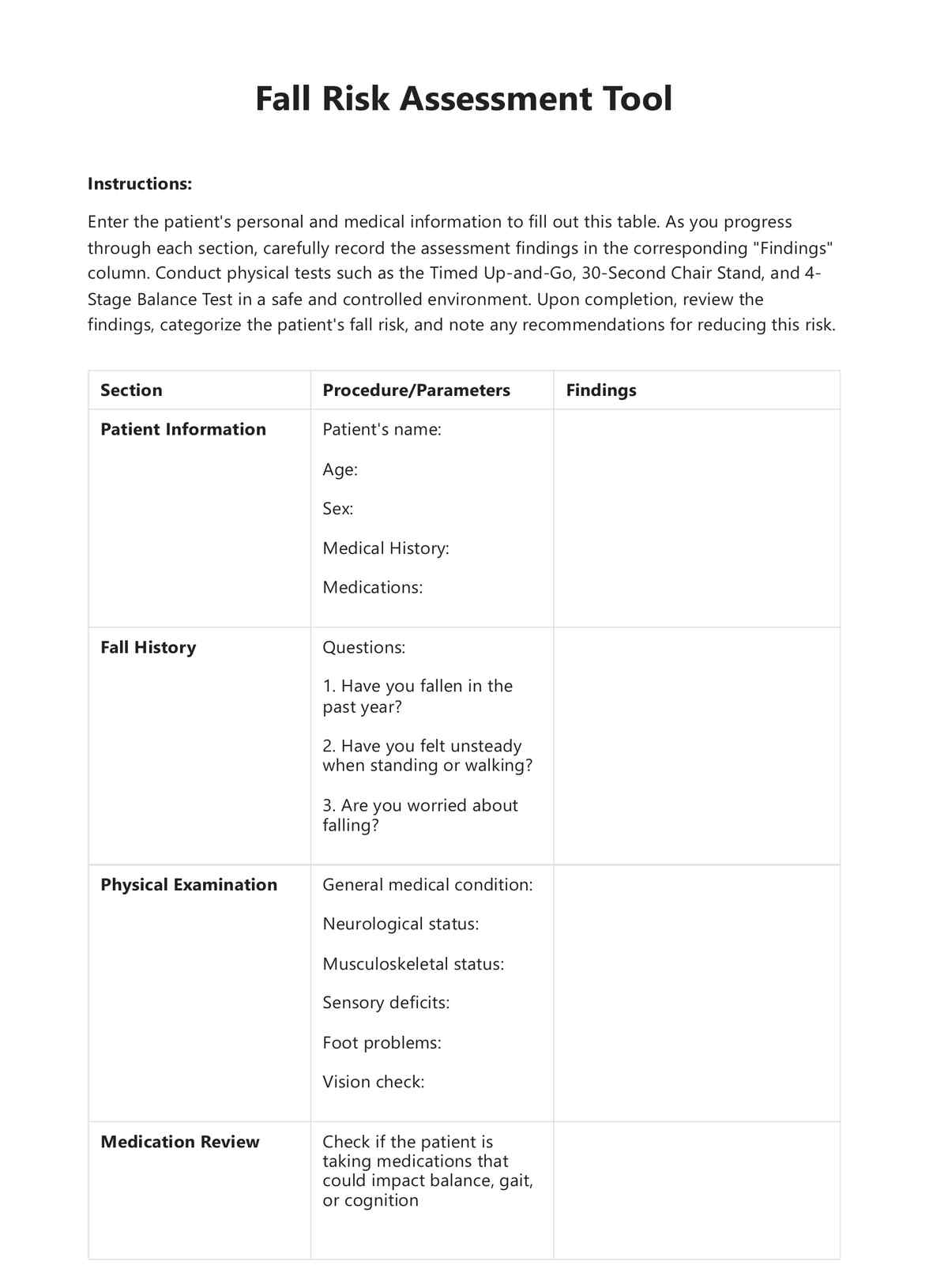
The assessment involves gathering patient information, reviewing fall history, conducting physical examinations, reviewing medications, evaluating gait and balance, and conducting an environmental assessment.
The assessment should be reviewed and updated regularly, especially if there's a significant change in the individual's health status or medication regimen. The CDC and American Geriatric Society recommend yearly assessments for all adults 65 and older.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











