Like with any clinical examination, there is some variation in how you choose to assess each Cranial Nerve Exam, but some things should remain constant every time you conduct an assessment. These include gathering the required equipment, checking the patient's name and date of birth, introducing yourself, explaining the examination in understandable language, and gaining consent to proceed.
Cranial Nerve Exam
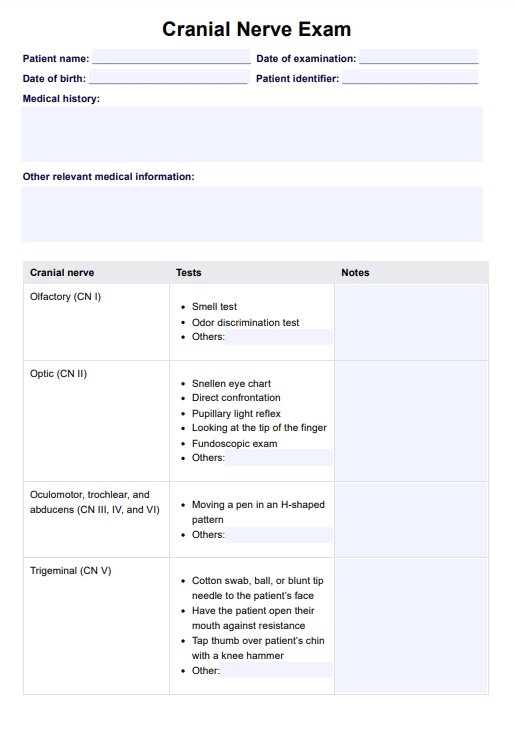
Use our Cranial Nerve Exam template as a guide when studying or conducting a cranial nerve assessment.
Cranial Nerve Exam Template
Commonly asked questions
Some contraindications to the Cranial Nerve Exam, such as facial trauma or swelling, may prevent proper assessment of CN III, CN IV, and CN IV. With advances in imaging technology, the results of a cranial nerve exam are no longer the sole method for diagnosing lesions. However, the cranial nerve exam remains an important part of the neurological exam and one that can be performed quickly with minimal equipment.
This will depend on the findings of the Cranial Nerve Exam. Following the Cranial Nerve Exam, further neurological testing, formal hearing assessments, speech examinations, or neuroimaging could follow.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











