People may self-harm as a way to cope with painful emotions, regulate difficult feelings, punish themselves, or seek relief from emotional numbness or dissociation. Self-harm is often associated with underlying mental health disorders.
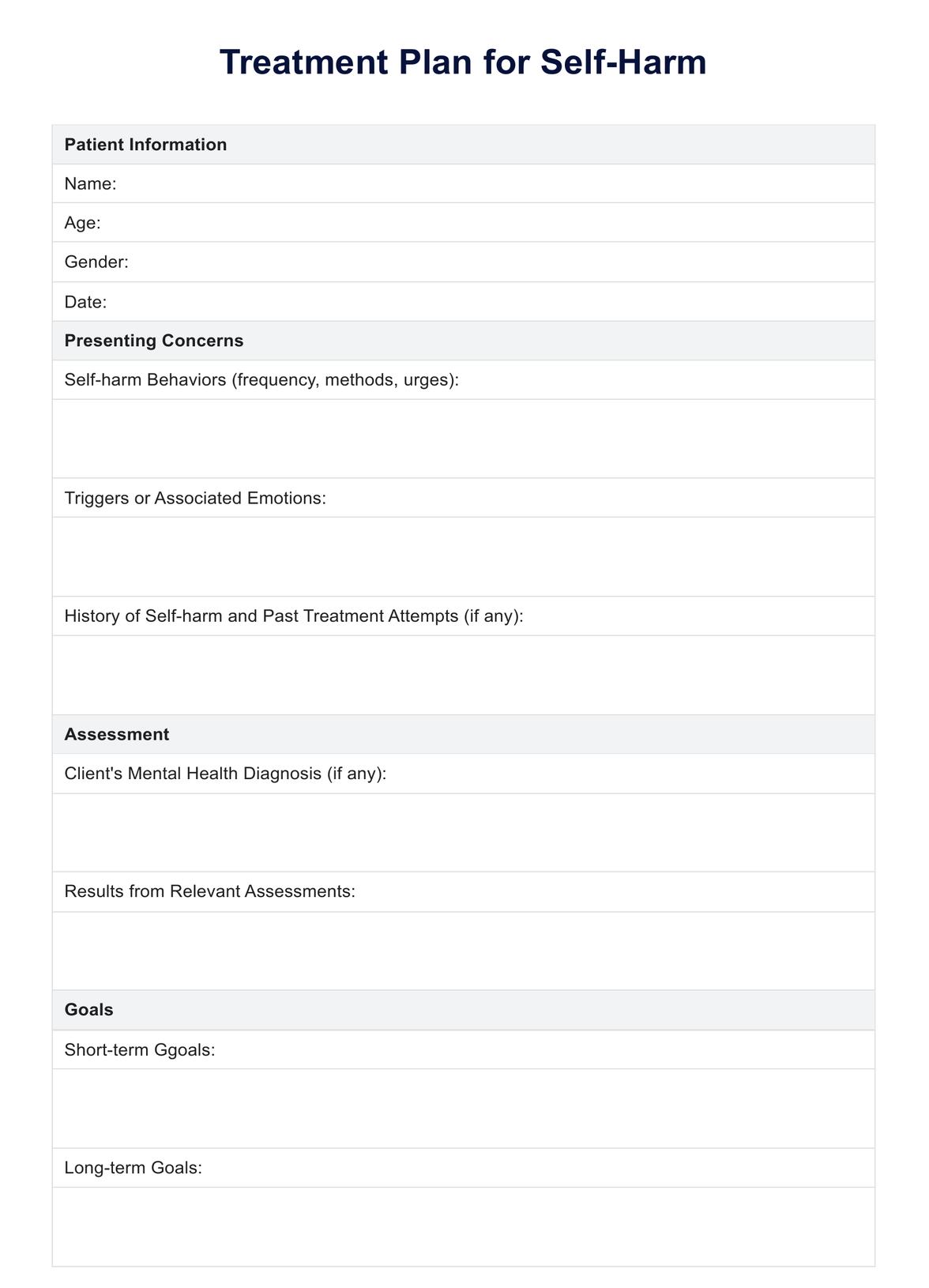
Treatment Plan for Self-Harm
Explore a helpful tool to help in safety planning and crisis management for clients engaging in self-harm and improve their health outcomes.
Treatment Plan for Self-Harm Template
Commonly asked questions
Harm reduction strategies aim to minimize the risk of injury and physical harm while working towards cessation of self-harming behaviors. These may include providing relaxation techniques and safe alternatives, teaching wound care, and developing a safety plan.
If you or someone you know is self-harming, it's important to seek professional help from a mental health provider, counselor, or therapist. In case of an emergency or if there is an immediate risk of harm, contact emergency services or a crisis hotline.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











