Pain medication refers to pharmaceutical drugs used to alleviate pain symptoms, while pain management encompasses a comprehensive approach to address pain, including medication, therapy, lifestyle changes, and other interventions to improve overall well-being and function.
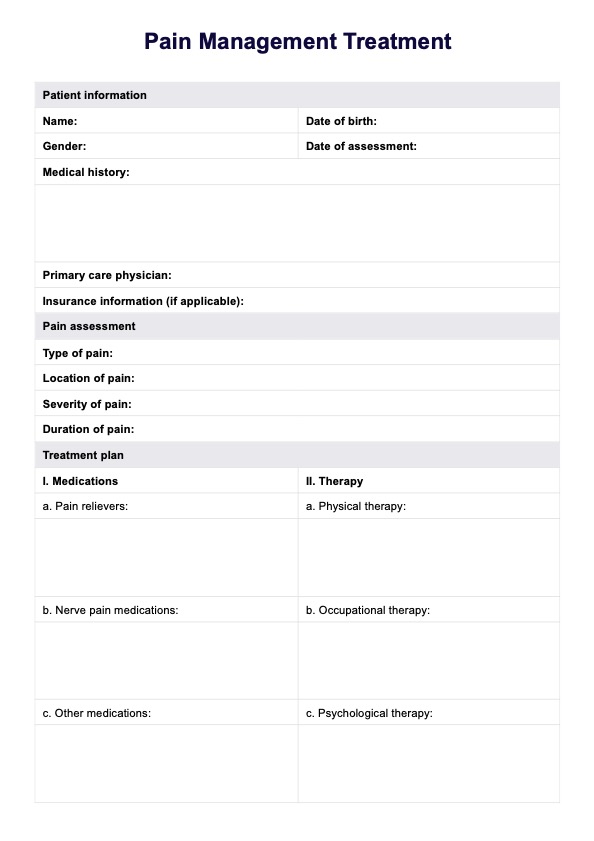
Pain Management Treatment
Discover effective pain management treatments and examples through Carepatron's free PDF download. Learn about various strategies to alleviate pain and improve your quality of life.
Pain Management Treatment Template
Commonly asked questions
Common causes of pain include injuries, medical conditions such as arthritis or fibromyalgia, nerve damage, surgery, inflammation, and psychological factors like stress or anxiety.
Discussing pain management options with patients fosters shared decision-making, empowers patients to take an active role in their care, and ensures treatments are tailored to their individual needs and preferences, leading to better outcomes and patient satisfaction.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











