A skin nursing assessment is a systematic evaluation of a patient's skin to identify any signs of damage, infection, or risk for conditions like pressure ulcers. It involves examining skin temperature, color, moisture, turgor, and integrity to ensure proper skin care and early intervention.
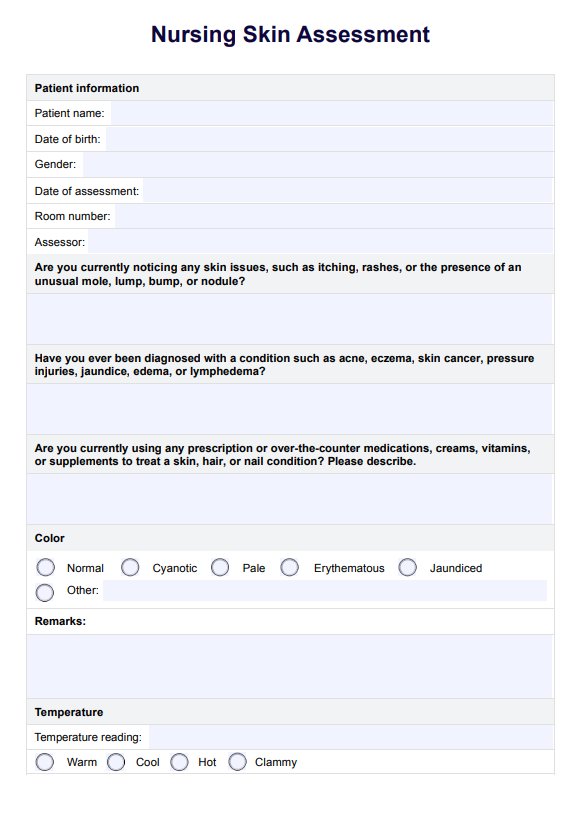
Nursing Skin Assessment
Learn the importance of nursing skin assessment, how to conduct it thoroughly, and document your findings with Carepatron's free PDF download.
Nursing Skin Assessment Template
Commonly asked questions
The five key elements of a skin assessment are temperature, turgor, color, moisture level, and skin integrity. These parameters help healthcare providers identify early signs of skin damage or other health issues affecting the skin.
To assess skin integrity, examine the skin for signs of damage, such as redness, lesions, tears, or blisters. Check for areas at risk, especially in bony prominences, and document any findings to guide treatment and prevention strategies.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











