While a cold primarily affects the nose and throat, bronchitis involves inflammation of the bronchial tubes in the lungs, leading to a persistent cough. Symptoms of a cold tend to be milder and resolve quicker than bronchitis.
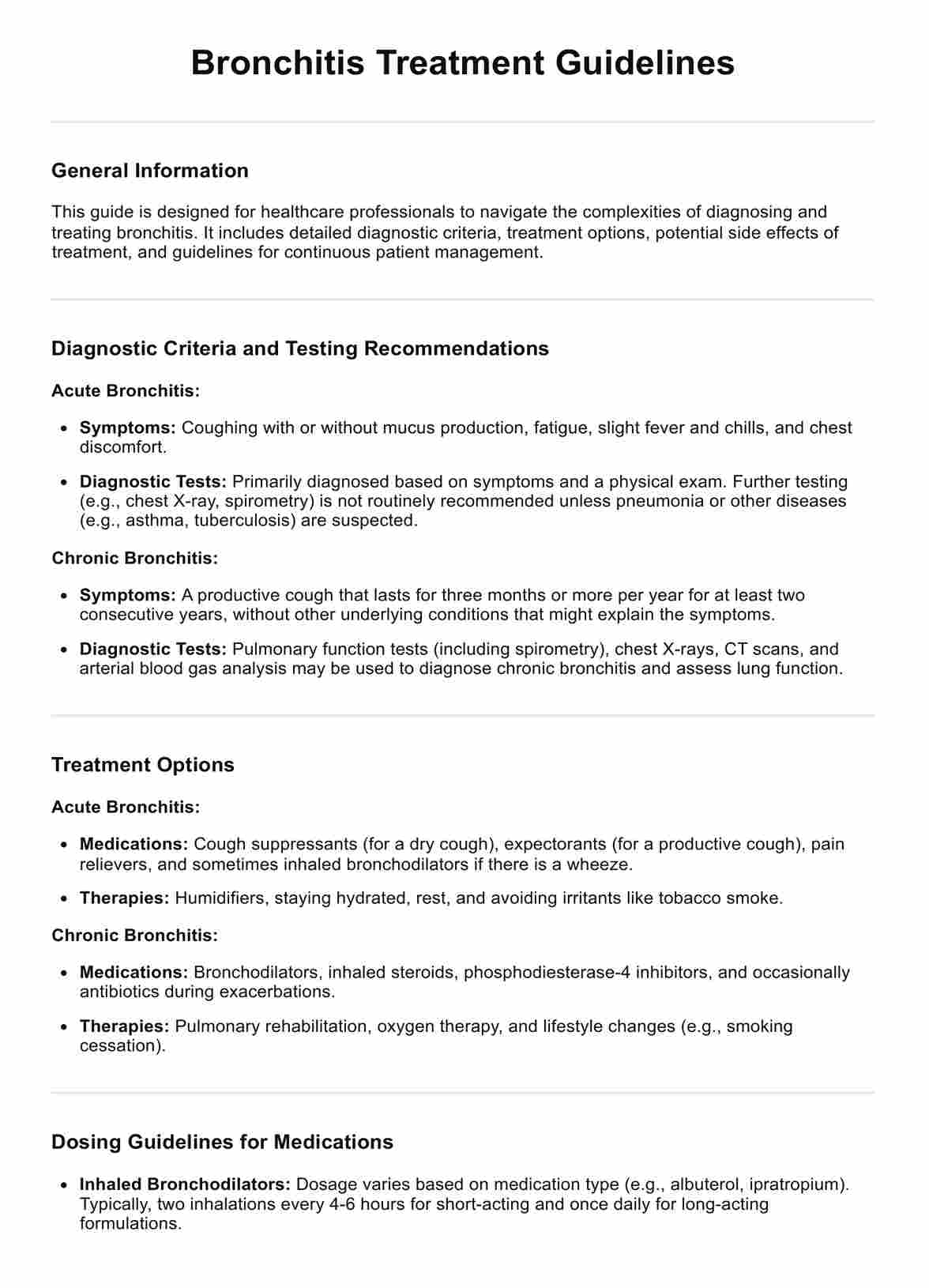
Bronchitis Treatment Guidelines
Explore bronchitis treatment guidelines for both acute and chronic forms, focusing on diagnosis, management, and preventive measures.
Bronchitis Treatment Guidelines Template
Commonly asked questions
Yes, especially in cases of acute bronchitis, if the infection spreads to the lungs, leading to pneumonia. However, this is more common among individuals with weakened immune systems, the elderly, or those with existing acute respiratory infections or conditions.
Acute bronchitis caused by viral infections can be contagious, similar to how colds and flu spread. Chronic bronchitis, linked to long-term irritation of the airways and not infections, is not contagious.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











