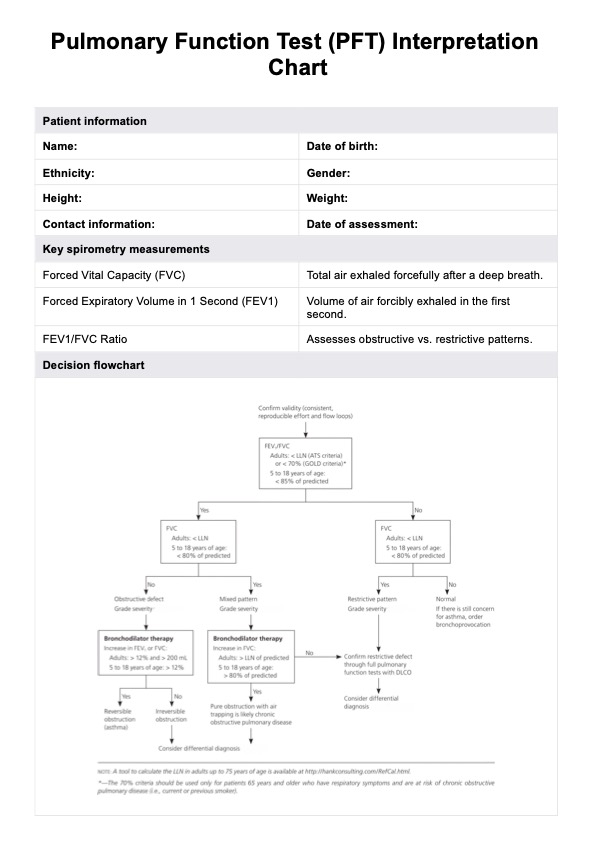
Interpret PFT results by analyzing key metrics such as FEV1, FVC, and the FEV1/FVC ratio, comparing them to predicted values and the lower limit of normal. These results help distinguish between obstructive lung disease, restrictive lung disease, or a mixed pattern.
PFT Interpretation Chart
Access Carpatron's free PFT Interpretation Chart PDF download to better understand pulmonary function test results.
PFT Interpretation Chart Template
Commonly asked questions
The FEV1/FVC ratio is often the most important value as it differentiates between obstructive and restrictive lung patterns. A ratio below 0.70 typically suggests obstructive lung disease, while a normal ratio with reduced FVC may indicate restriction.
A "bad" result includes values significantly below predicted levels, such as an FEV1/FVC ratio under 0.70 or an FVC below 80% of predicted. These findings may indicate severe respiratory disease or impaired lung function requiring further investigation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











