What is a Nursing Discharge Note?
A Nursing Discharge Note is an essential document in the healthcare field. It is a comprehensive record summarizing a patient's hospital stay from admission to discharge and detailing their health status and treatment plans. Created by a qualified nurse, these notes are a critical component of the healthcare communication system, providing essential information for future care planning and enabling a seamless transition from hospital care to home or another healthcare facility.
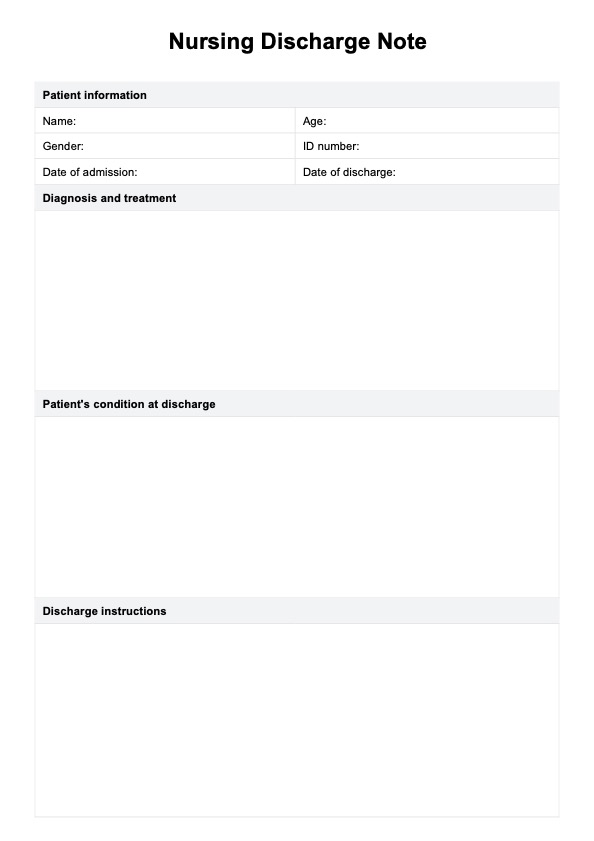
The depth and breadth of information captured in a discharge nursing note make it an indispensable tool for patient care. It encapsulates many elements, including the patient's identification, the diagnoses made during the stay, the treatments administered, and the patient's condition at discharge. It also outlines the instructions for the patient's care after leaving the facility, medication details, and plans for any follow-up care.
Discharge nursing notes also help educate the patient and their family about their health condition, the importance of medication adherence, and any potential signs or symptoms that need to be monitored post-discharge. It is a roadmap for the patient's healthcare journey beyond the hospital, providing the necessary guidelines for continuous and effective care.
From a broader perspective, discharge nurses' notes aid in individual patient care and contribute to the more extensive healthcare system. They provide valuable data for research, help identify trends, and can be used to enhance patient care protocols and hospital discharge processes.
Despite being a single document, discharge nursing notes have a manifold and far-reaching impact, underlining their crucial role in successful patient recovery and overall healthcare management. Continue reading our guide, and you will see a discharge nursing note example.