Lupus is identified through clinical findings such as skin rashes, nasal ulcers, joint pain, and organ involvement, along with laboratory markers like antinuclear antibodies and c-reactive protein levels. A confirmed diagnosis requires meeting established diagnostic criteria, including a combination of symptoms, hematologic abnormalities, and immunologic tests.
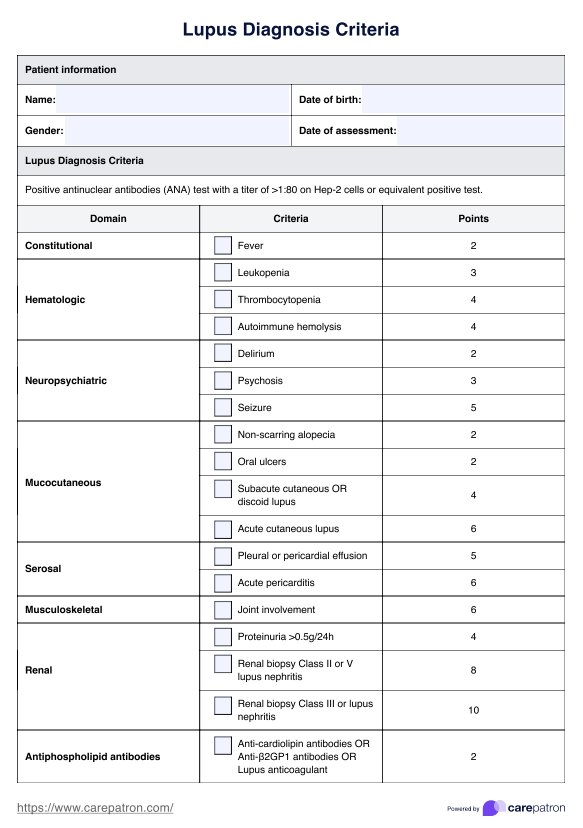
Lupus Diagnosis Criteria
Access Carepatron's free Lupus Diagnosis Criteria PDF and understand key clinical indicators and support accurate assessments with essential resources.
Lupus Diagnosis Criteria Template
Commonly asked questions
The four main types of lupus are systemic lupus erythematosus (SLE), cutaneous lupus erythematosus, drug-induced lupus, and neonatal lupus. SLE patients experience multi-organ involvement, while cutaneous lupus primarily affects the skin, and drug-induced lupus resolves after stopping the triggering medication.
Lupus has no cure, but early disease detection and targeted management can control symptoms and prevent complications. Treatment focuses on suppressing the immune response, reducing inflammation, and addressing organ-specific damage, such as renal disorders and hematologic abnormalities.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











