Fall Risk Assessment is particularly important for older adults, individuals with mobility impairments, those with a history of falls, and patients recovering from injuries or surgeries that affect mobility.
Fall Risk Assessment
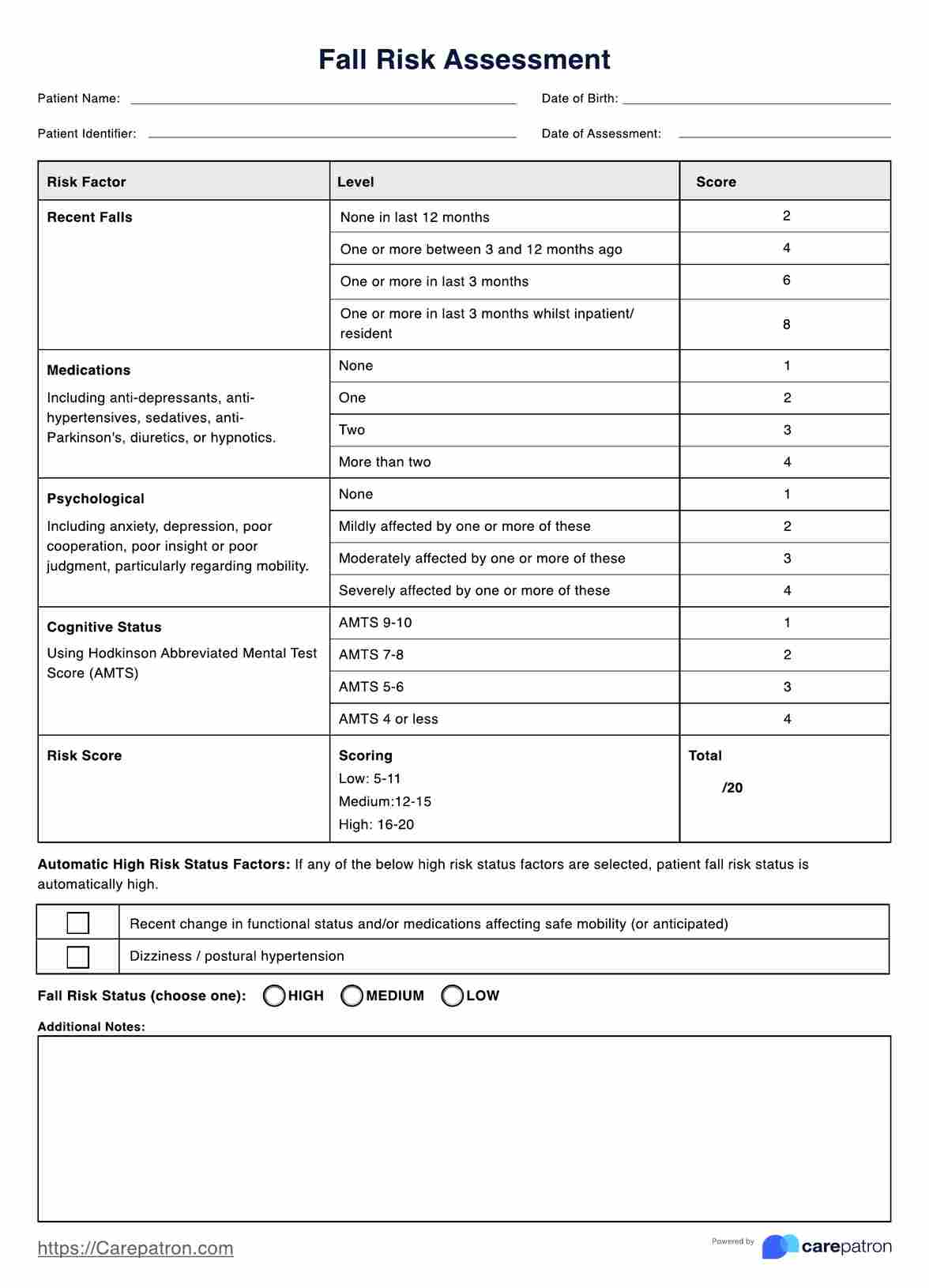
Identify patients who may be at risk of a fall and implement interventions to prevent falls before they happen, with our simple Fall Risk Assessment, based on the Peninsula Health FRAT.
Fall Risk Assessment Template
Commonly asked questions
Common risk factors assessed in the Fall Risk Assessment include previous falls, balance impairment, medication usage (sedatives or antihypertensives), cognitive impairment, visual deficits, and environmental hazards.
Fall Risk Assessment is typically conducted using standardized assessment tools, questionnaires, and physical examinations. Healthcare professionals may also review medical records, conduct medication reviews, and assess the individual's home environment for potential fall hazards.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











