The biopsychosocial-spiritual model is a holistic framework that recognizes the interconnectedness of various factors influencing an individual's health.
Biopsychosocial Spiritual Model
Explore holistic well-being with our guide on the biopsychosocial-spiritual model—unlocking insights to enhance health on every level.
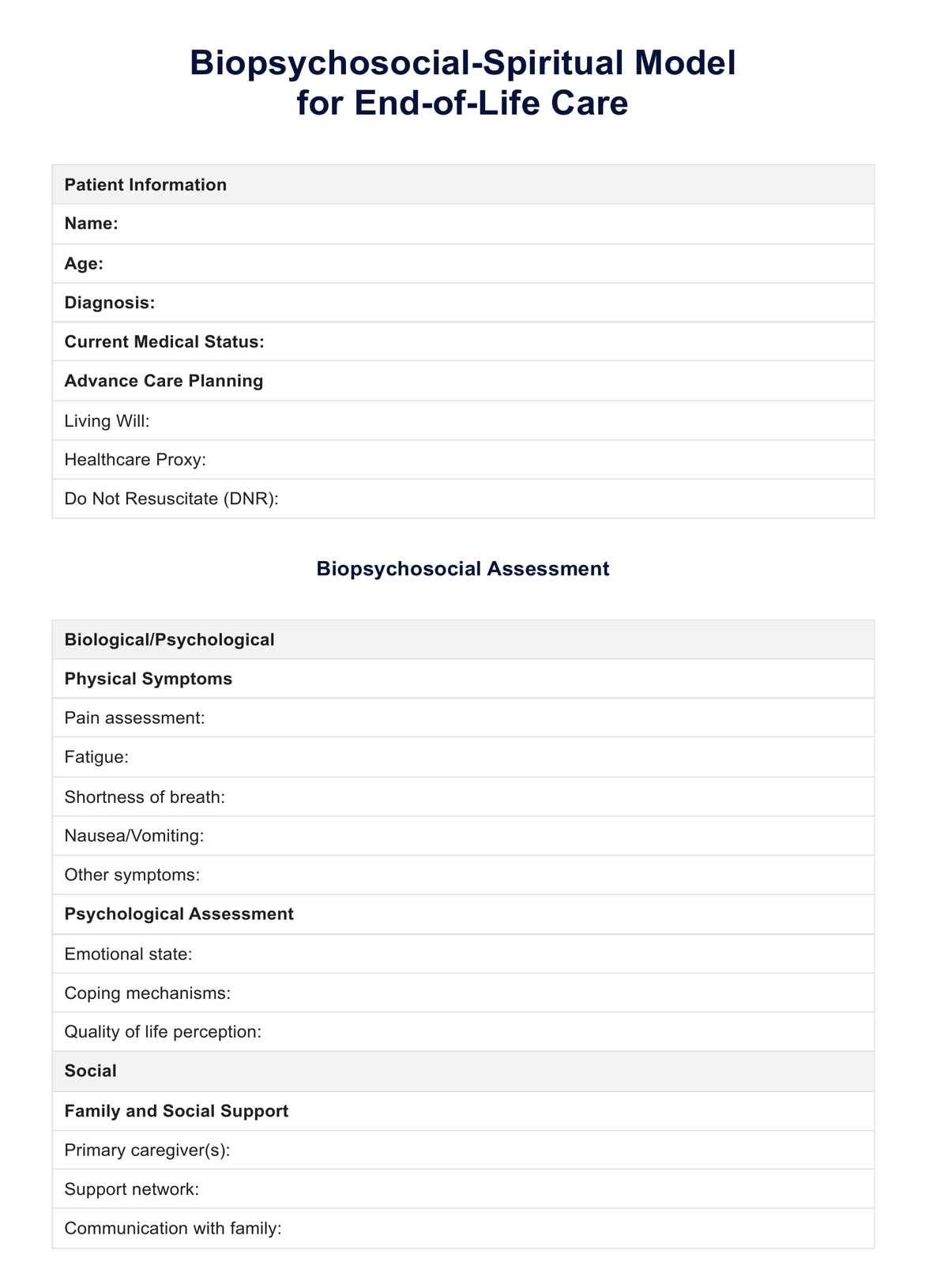
Biopsychosocial Spiritual Model Template
Commonly asked questions
Spirituality is essential for overall health as it acknowledges belief systems, values, and a sense of meaning or purpose in an individual's life. Addressing spiritual needs can provide a more comprehensive understanding of an individual's experiences and challenges.
The biopsychosocial-spiritual model considers various factors that affect health issues. It encourages a patient-centered approach to healthcare, where healthcare providers consider biological, psychological, social, and spiritual aspects when treating patients.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











