The SIT Scale is designed to measure the impact of self-injurious behavior on individuals in terms of trauma. It assesses the psychological and emotional consequences of engaging in self-harm, providing insights into the severity of trauma associated with self-injury. Mental health professionals use the SIT Scale to inform treatment planning, intervention strategies, and progress monitoring in individuals who engage in self-harming behaviors.
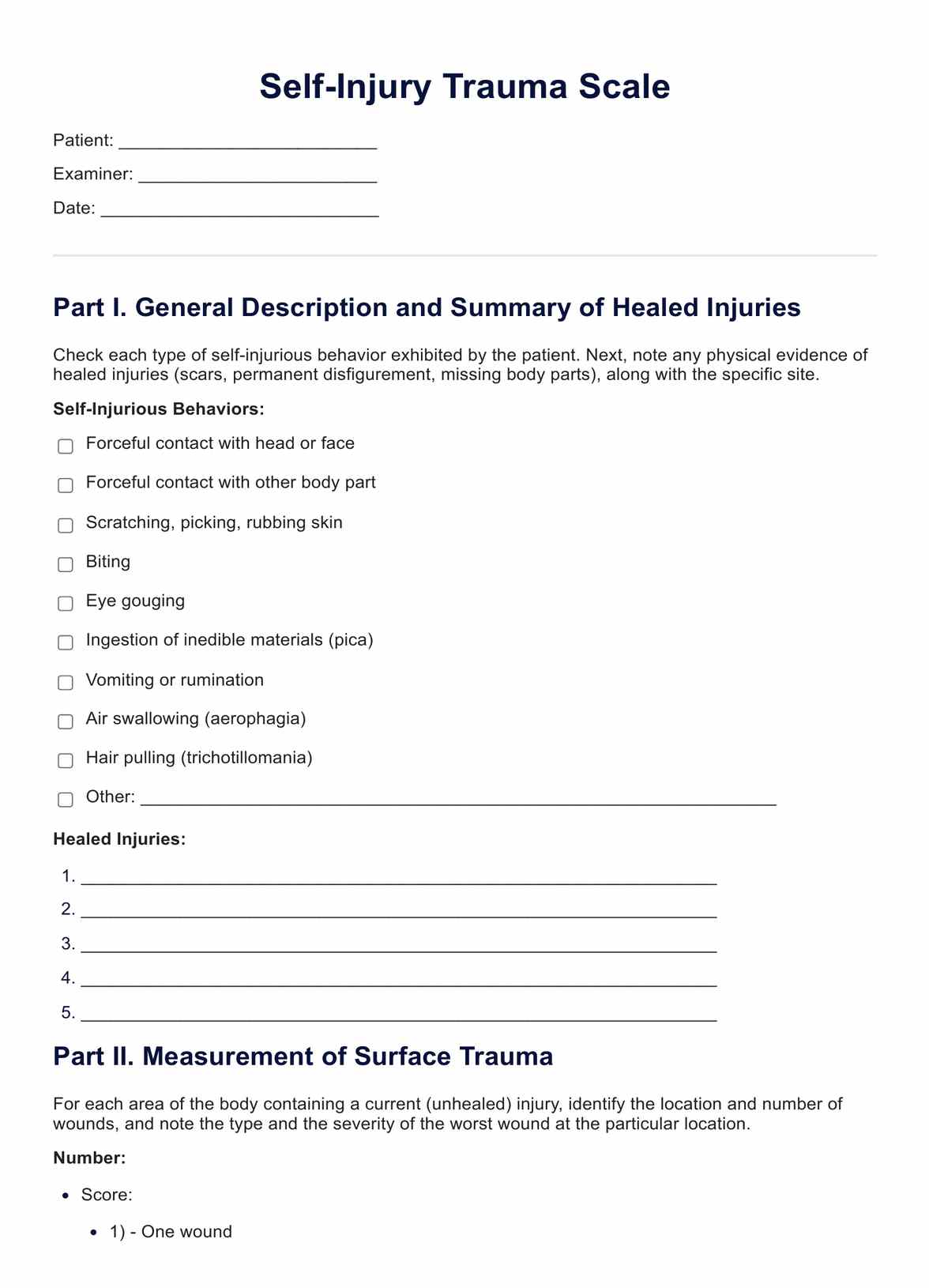
Self Injury Trauma Scale
Explore the Self Injury Trauma Scale: Understanding, assessing, and navigating the path to healing from self-harm and associated trauma.
Self Injury Trauma Scale Template
Commonly asked questions
The scoring of the SIT Scale is typically based on a set of guidelines provided by the test developers. Specific criteria assign scores to individual responses, which are then aggregated to generate a total score. Higher scores generally indicate a more significant impact of self-injury-related trauma.
No, the SIT Scale is not a diagnostic tool on its own. Instead, it is an assessment instrument used by mental health professionals to gather information about the psychological and emotional impact of self-injury. While the scale provides valuable insights into the individual's experiences, a diagnosis typically involves a comprehensive clinical evaluation considering multiple factors.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











