The primary nursing goals for bed sores are to promote wound healing, prevent further skin breakdown, relieve pain, and educate the patient on preventive measures. These goals focus on maintaining skin integrity and minimizing the risk of infection.
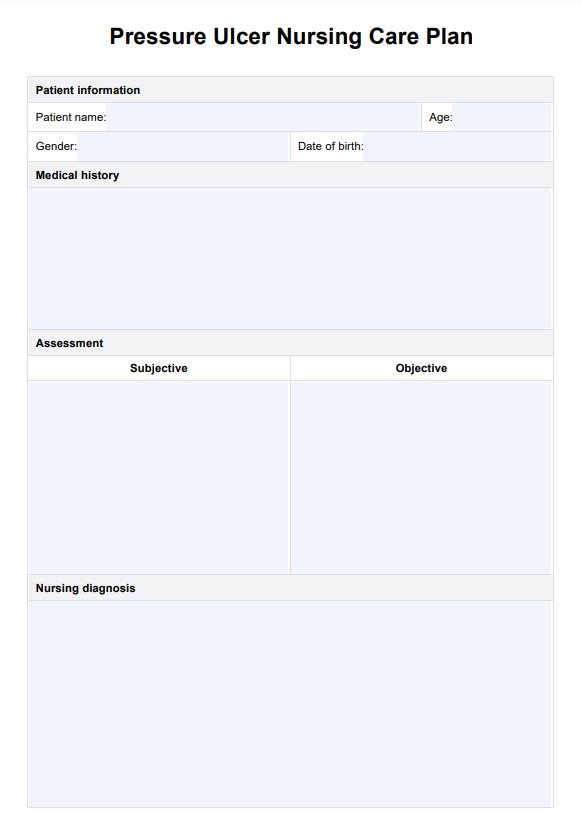
Pressure Ulcer Nursing Care Plan
Use this guide to create pressure ulcer and injury nursing care plans to deliver superior care and prevention.
Pressure Ulcer Nursing Care Plan Template
Commonly asked questions
Nursing interventions for a pressure ulcer include repositioning the patient every two hours, using specialized support surfaces (e.g., foam or air-filled mattresses), ensuring proper nutrition and hydration, providing negative pressure wound therapy for advanced ulcers, and maintaining strict hygiene practices to prevent infection.
Nursing management can prevent developing pressure injuries by conducting regular skin assessments, repositioning patients frequently to relieve pressure, maintaining proper hygiene, using pressure-relieving devices, and ensuring adequate nutrition and hydration to support skin health.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











