If a therapy assistant (PTA or OTA) provides at least 10% of a timed service, you must use the CQ or CO modifier when billing Medicare or any insurance company that follows Medicare billing guidelines to indicate the assistant's involvement.
Medicare 8-minute Rule Chart
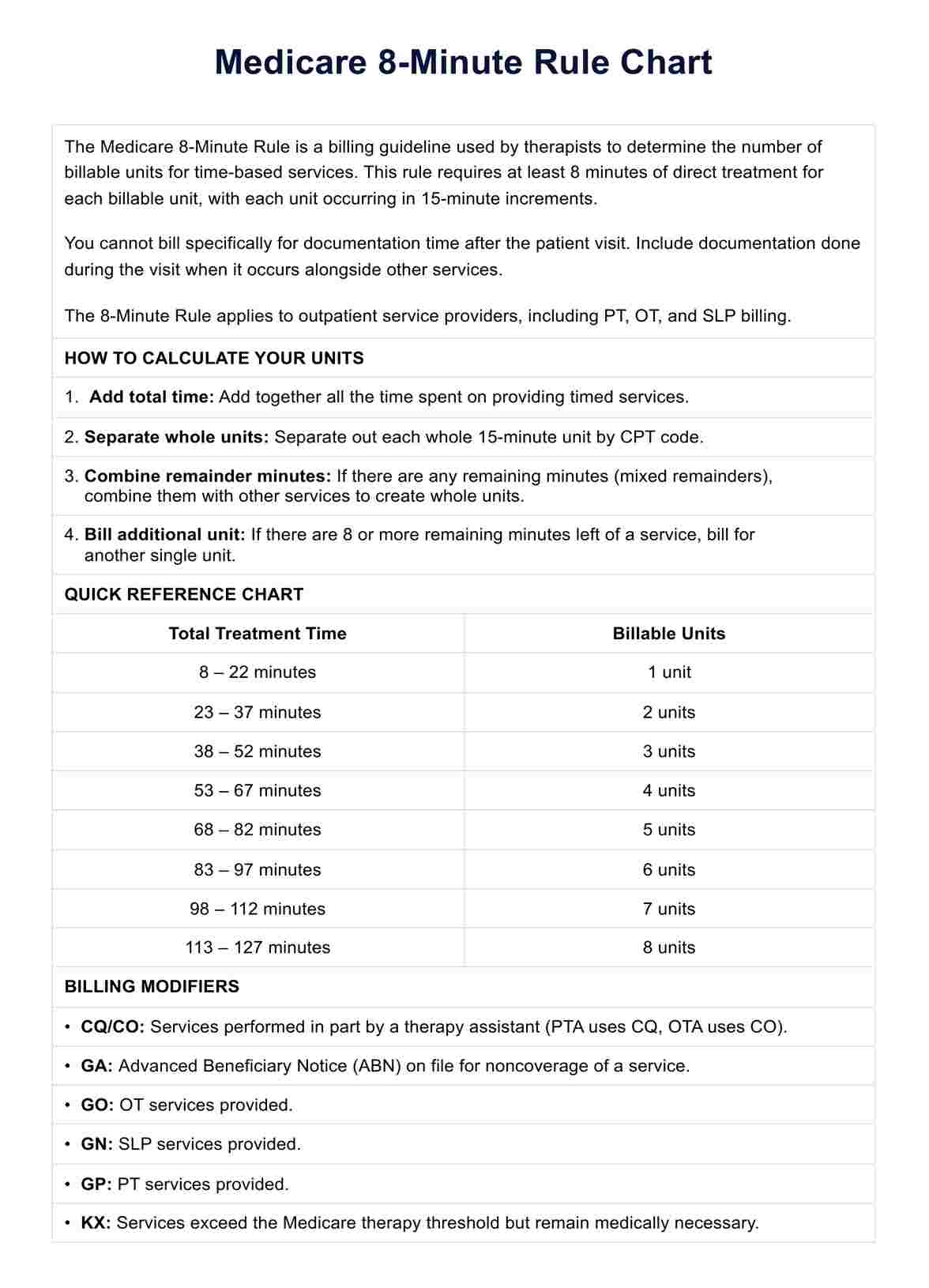
Master the Medicare 8-Minute Rule with our comprehensive chart and guide. Simplify billing for time-based therapy services and maximize reimbursement.
Use Template
Medicare 8-minute Rule Chart Template
Commonly asked questions
Many private insurance companies and Medicaid programs adopt Medicare billing guidelines, including the 8-Minute Rule, for consistency in billing practices across different payers.
The Medicare 8-Minute Rule is crucial for physical therapy billing because it ensures that therapy services are billed accurately based on the actual time spent providing treatment, preventing overbilling and ensuring fair reimbursement.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











