The dysphagia care plan aims to improve impaired swallowing related to function, maintain adequate nutrition, prevent aspiration pneumonia, and enhance the patient's overall quality of life.
Dysphagia Care Plan
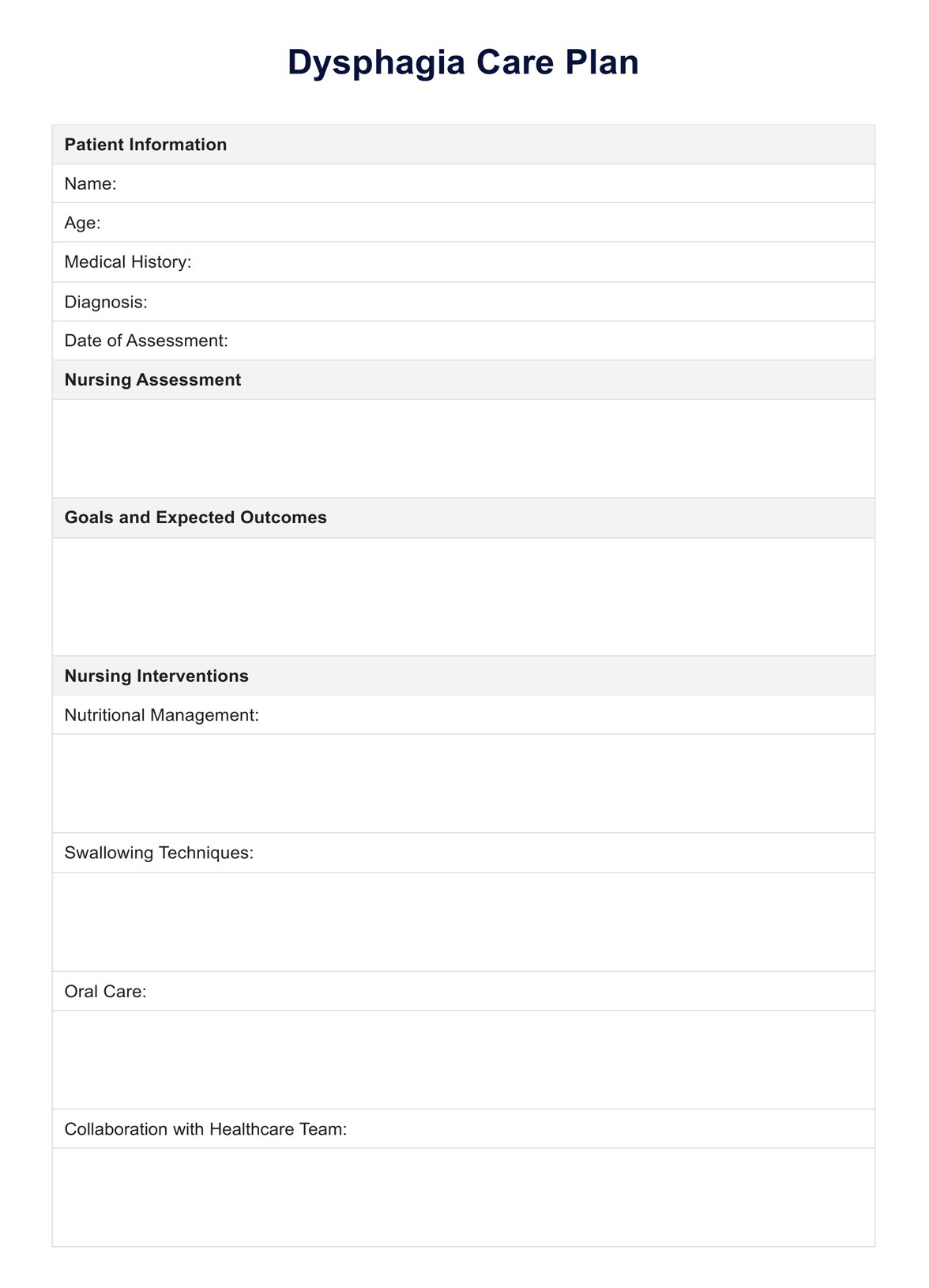
Optimize patient outcomes with our free Dysphagia Care Plan template. Streamline care delivery for individuals with swallowing difficulties.
Dysphagia Care Plan Template
Commonly asked questions
Interventions for dysphagia include modifying diet texture, implementing swallowing techniques, providing oral care, coordinating with other healthcare professionals, and monitoring the patient's progress.
The four stages of dysphagia are the oral preparatory phase, the oral phase, the oral cavity, the pharyngeal phase, and the esophageal phase. These stages represent the events involved in swallowing, from chewing and forming a bolus to passage through the throat and into the esophagus.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











