Healthcare providers, including doctors, nurses, and specialists, typically request Blood Differential Tests to diagnose and monitor various medical conditions.
Blood Differential
Discover the importance of Blood Differential Tests in healthcare. Learn about their uses, results, and significance in diagnosing medical conditions.
Use Template
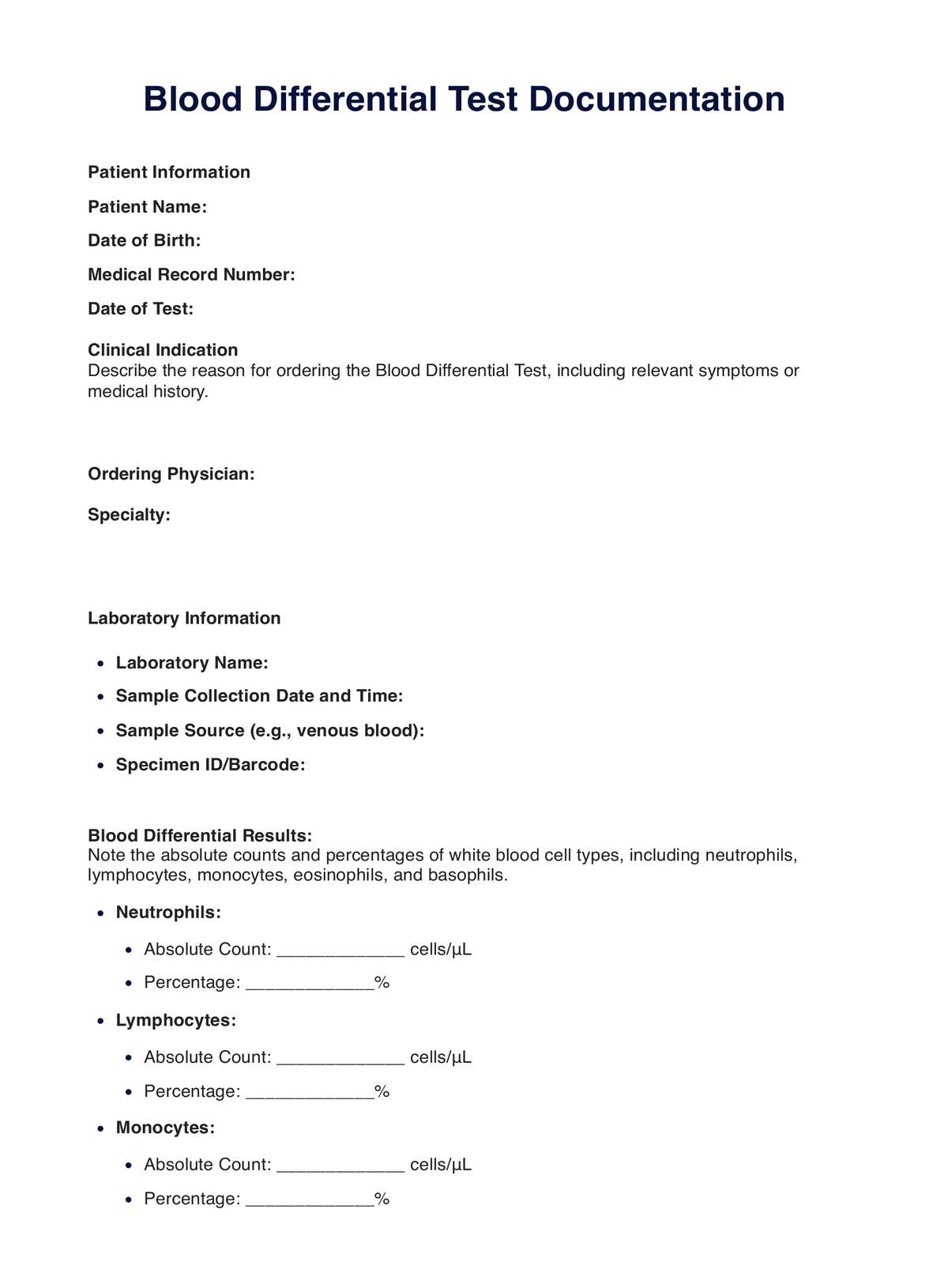
Blood Differential Template
Commonly asked questions
Blood Differential Tests are used when there's a suspicion of infection, blood disorders, or autoimmune diseases or to monitor response to treatments like chemotherapy.
A Blood Differential Test involves analyzing a blood sample to count and classify different types of white blood cells, providing insights into a patient's health and potential medical conditions.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











