It depends on the person being assessed. This assessment tries to gauge heavy and serious topics, so don’t expect to accomplish the whole thing in just a few minutes.
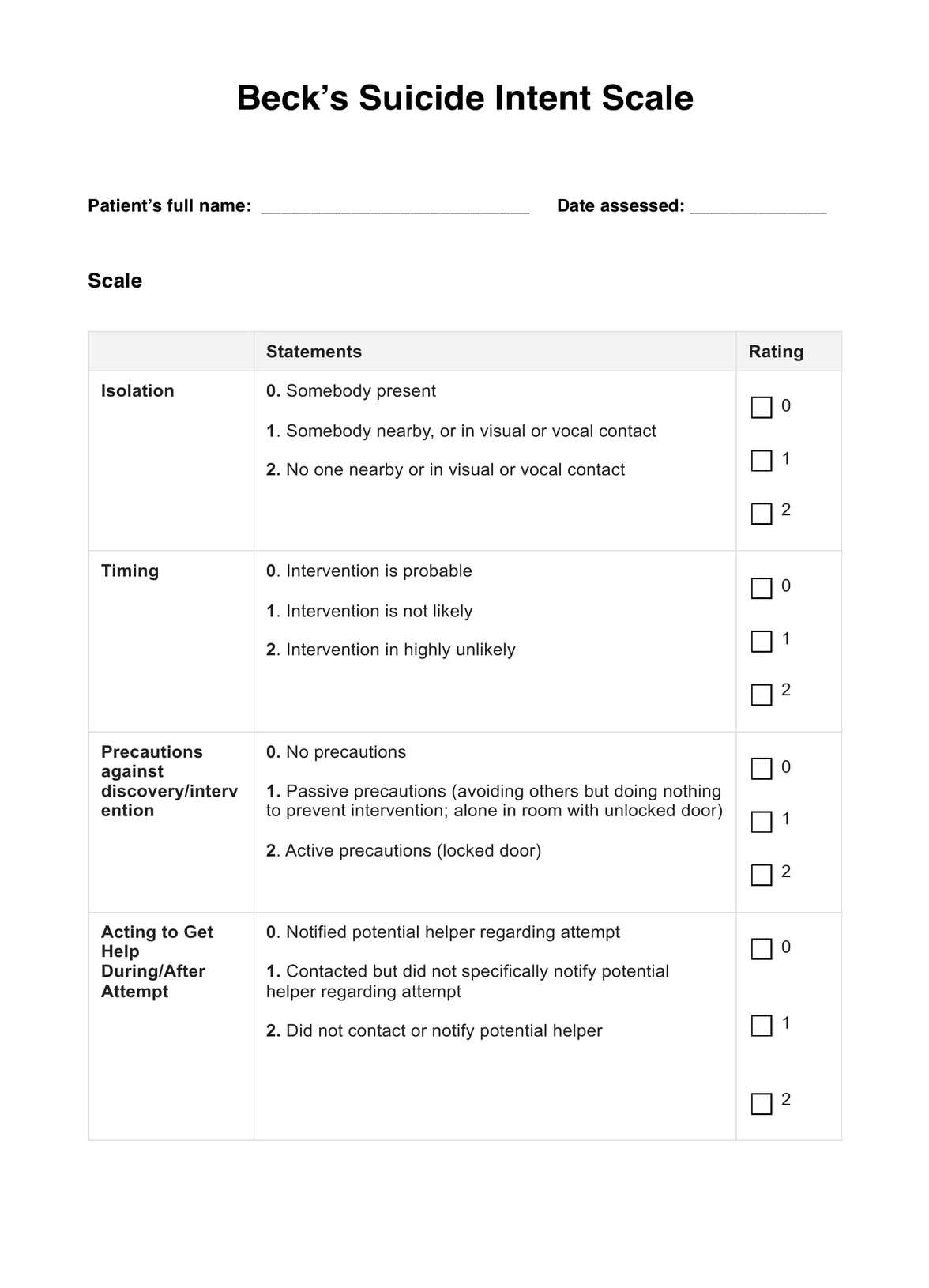
Beck’s Suicide Intent Scale
Assess the suicide risk of your patient by using Beck’s Suicide Intent Scale. Learn more about it through this guide.
Beck’s Suicide Intent Scale Template
Commonly asked questions
It also depends on the person being assessed. Some patients might find it difficult to answer your questions because suicide ideation and intent is a touchy subject and quite difficult to talk about. So make your patient comfortable enough to answer your questions.
If you somehow managed to find this guide and you’re not a professional, you can definitely download the template and answer it for yourself, but please don’t diagnose yourself with anything. If you have thoughts about suicide, whether you plan on acting it out or not, please see a professional for help.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











