ADL coding provides a categorical system for physicians, nurses, and other care providers to assess a patient's ability to perform various essential activities of daily living (ADLs). It helps assess a patient's functional status and need for assistance in basic daily tasks, which is crucial for care planning.
ADL Coding Cheat Sheet
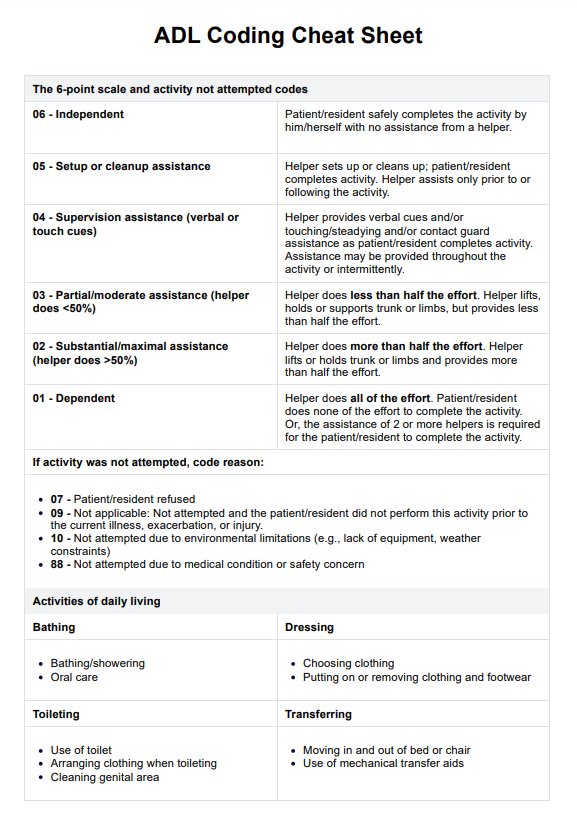
Discover our ADL Coding Cheat Sheet, an essential tool for healthcare professionals to assess and document patients' daily activities efficiently.
Use Template
ADL Coding Cheat Sheet Template
Commonly asked questions
The rule of 3 in ADL coding refers to categorizing ADLs based on the level of assistance needed: independent (no help), some help (up to two times), and dependent (three or more times or total assistance).
ADLs are scored based on the patient's level of independence from 0 to 6. A higher score indicates a greater ability to perform that activity independently. Scoring criteria vary depending on the specific ADL coding system.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











