Nutrition directly influences mental health by affecting brain function and neurotransmitter activity. A diet rich in essential nutrients like omega-3 fatty acids, vitamins, and minerals supports brain health, enhances mood, and can reduce the symptoms of mental health conditions such as depression and anxiety. Conversely, diets high in processed foods and sugar can worsen mental health symptoms.
Nutrition and Mental Health
Learn how nutrition impacts mental health. Explore key nutrients, the gut-brain axis, and dietary patterns to support mood and cognitive well-being.
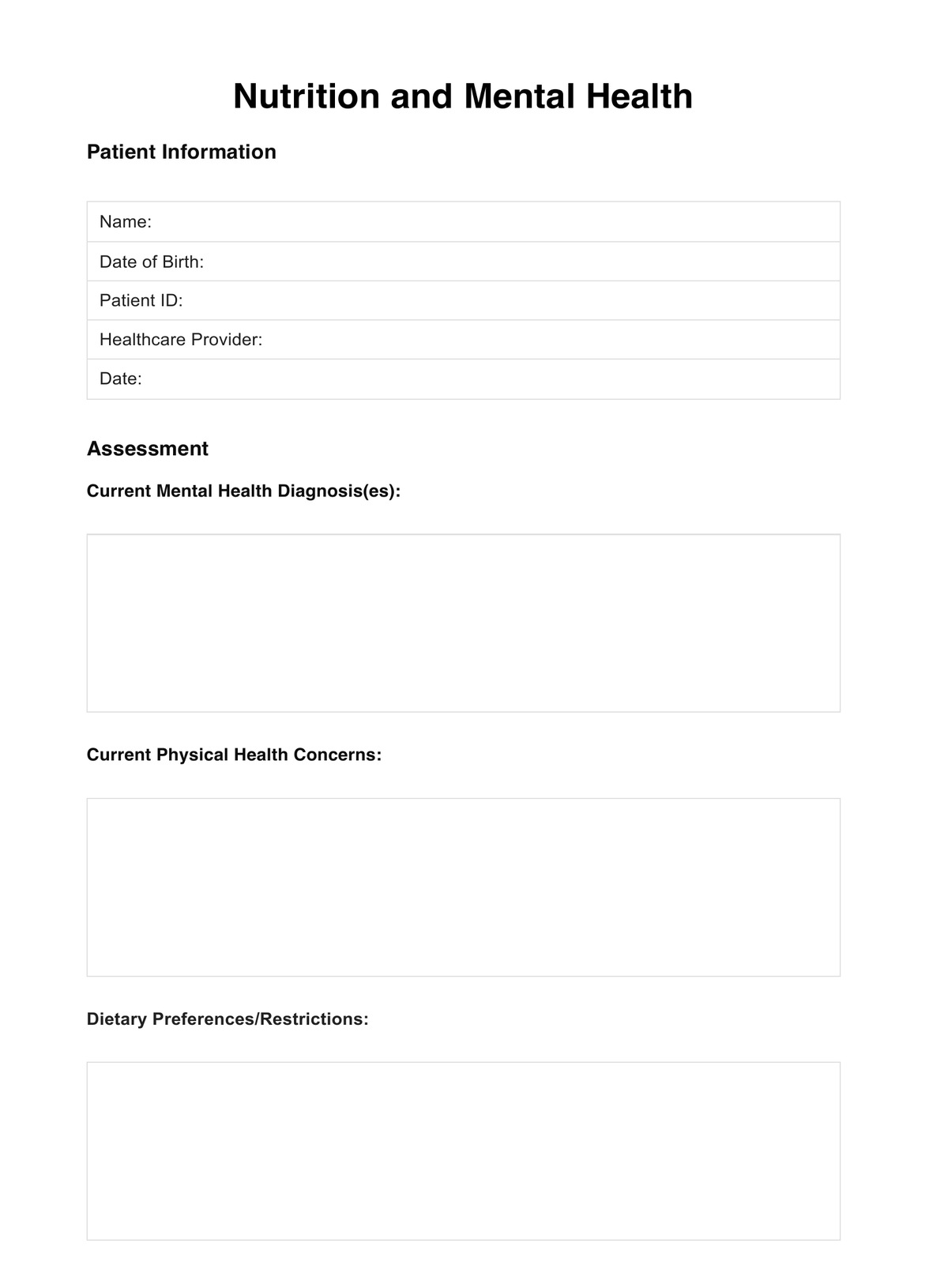
Nutrition and Mental Health Template
Commonly asked questions
Nutrition care is pivotal in managing and potentially improving mental health conditions by ensuring the body receives the necessary nutrients to support brain function and mental well-being. It involves tailored dietary advice to address nutritional deficiencies, improve gut health, and promote overall brain health, contributing to alleviating mental health symptoms and enhancing treatment outcomes.
Foods that balance mental health include those rich in omega-3 fatty acids (such as salmon and flaxseeds), antioxidants (found in berries and leafy greens), and probiotics (in yogurt and fermented foods). Whole grains, lean proteins, and fruits and vegetables provide essential vitamins, minerals, and amino acids supporting brain function and mood regulation.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











