Even if your symptoms don't fully align with the diagnostic criteria for mood disorders, it's crucial to seek professional help. There are also further categories for mood disorders as well such as unspecified bipolar disorder and unspecified depressive disorder, which may account for this. Many people experience subthreshold symptoms that can still significantly affect their lives and may benefit from treatment or intervention.
List of Mood Disorders
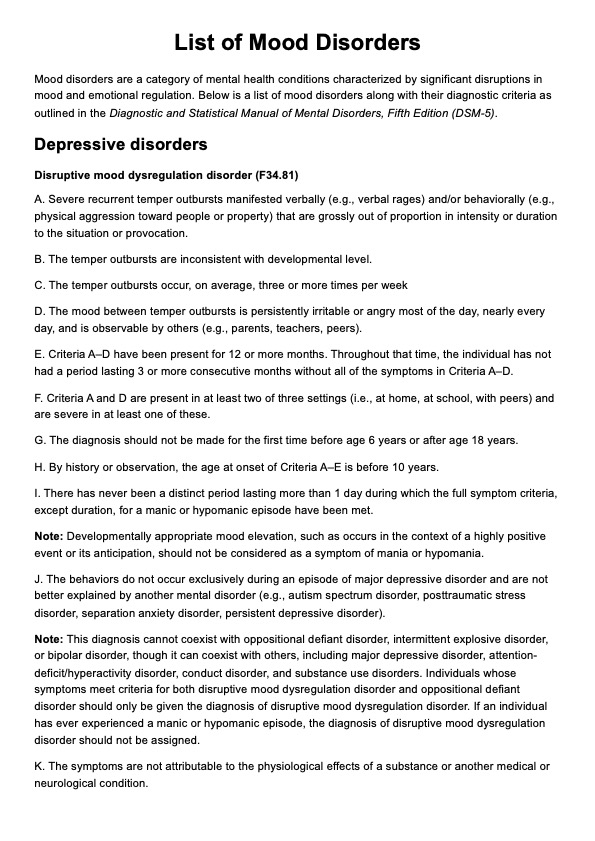
Use our List of Mood Disorders as a quick reference of symptoms to help clients going through these challenges.
List of Mood Disorders Template
Commonly asked questions
A mood disorder due to a general medical condition is a diagnosis given when a significant mood disturbance results directly from the physiological effects of a separate medical condition. This diagnosis underscores the direct link between the medical condition and the mood disorder symptoms.
Substance-induced mood disorders are specific types of mental health conditions characterized by depressive, anxiety, psychotic, or manic symptoms that directly result from the physiological effects of substance use, including prescription medications, illegal drugs, and alcohol. These disorders can manifest during active substance use, intoxication, or withdrawal phases.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











