Endocrine Assessment
Explore comprehensive insights into endocrine disorders, including thyroid, adrenal, and pituitary issues, and their management and treatment options.


What is an Endocrine Assessment?
An endocrine assessment is a comprehensive evaluation of the endocrine system, which includes various glands in the body that produce hormones. These hormones regulate many of the body's functions, including metabolism, growth and development, tissue function, and mood.
The assessment focuses on identifying any dysfunctions within the endocrine system, which could manifest as thyroid gland issues, pituitary gland abnormalities, adrenal insufficiency, or other hormone-related disorders such as diabetes mellitus, polycystic ovary syndrome, and thyroid disease.
Understanding the importance of being tested is crucial, as many endocrine disorders can have significant, sometimes life-altering effects on a patient's health. Early detection and diagnosis of conditions like thyroid dysfunction, growth hormone deficiency, or congenital adrenal hyperplasia can lead to more effective management and treatment strategies, potentially minimizing the long-term impacts of these disorders.
Endocrine assessments help pinpoint risk factors and identify the endocrine disorder's specific nature, facilitating a targeted approach to treatment, which may include hormone replacement therapy or interventions for conditions like primary adrenal insufficiency.
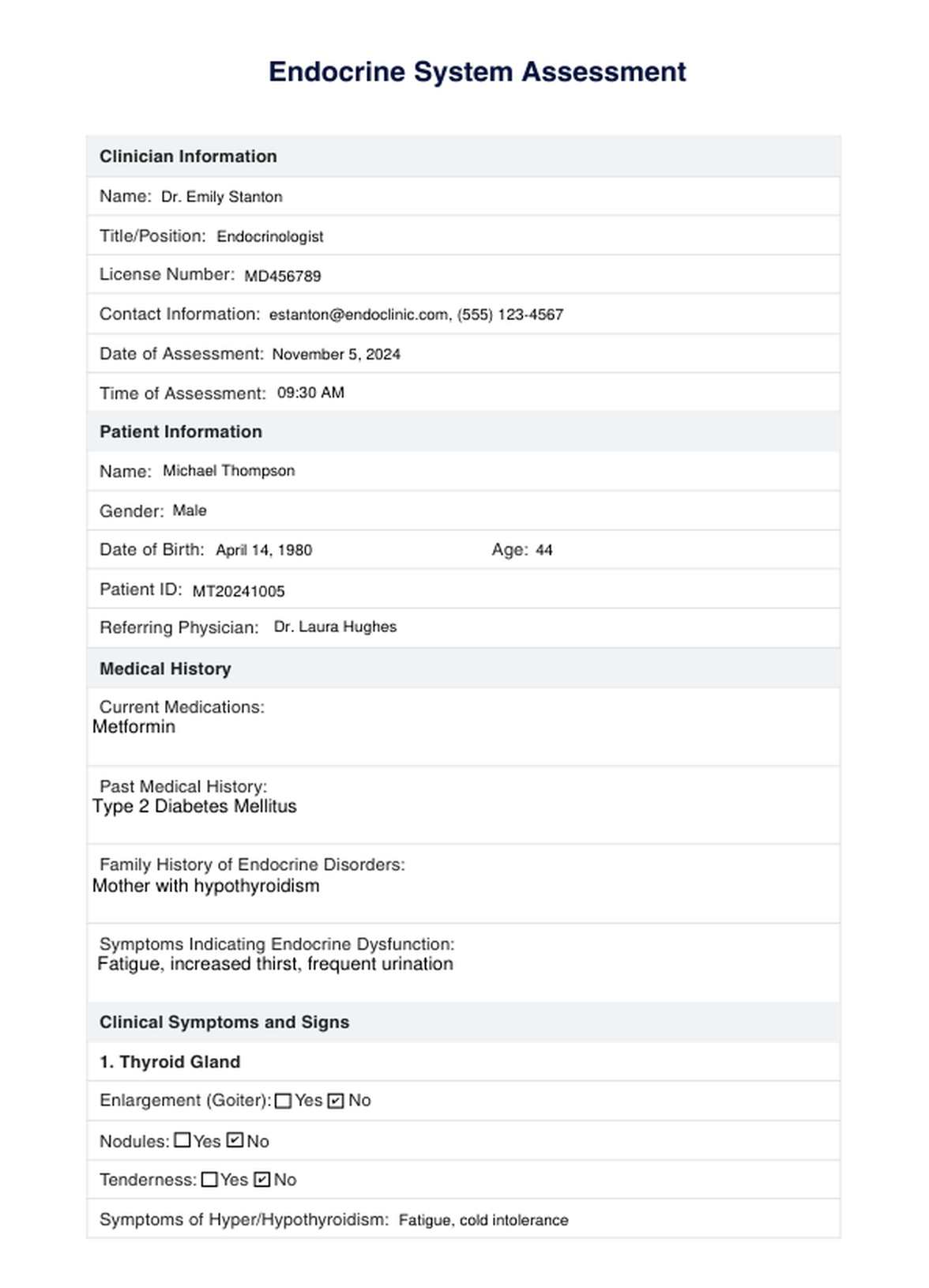
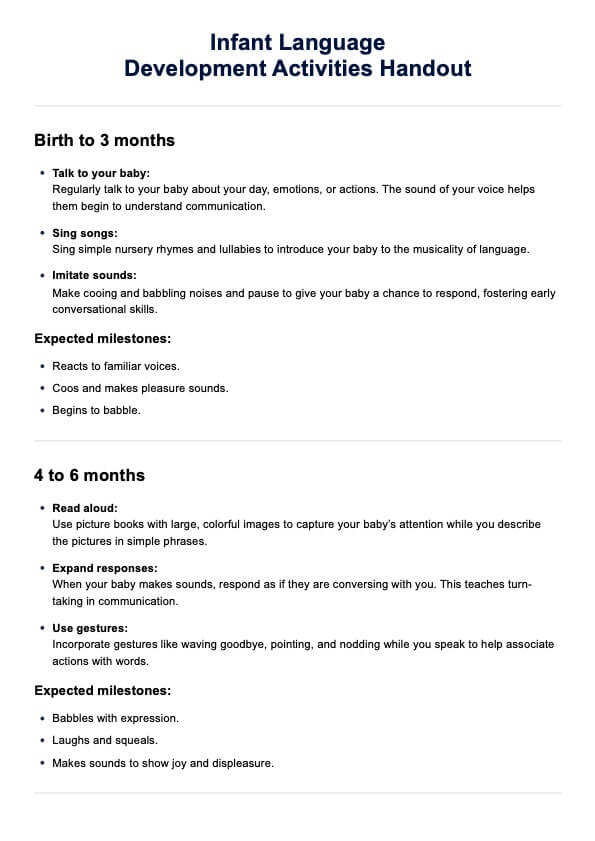
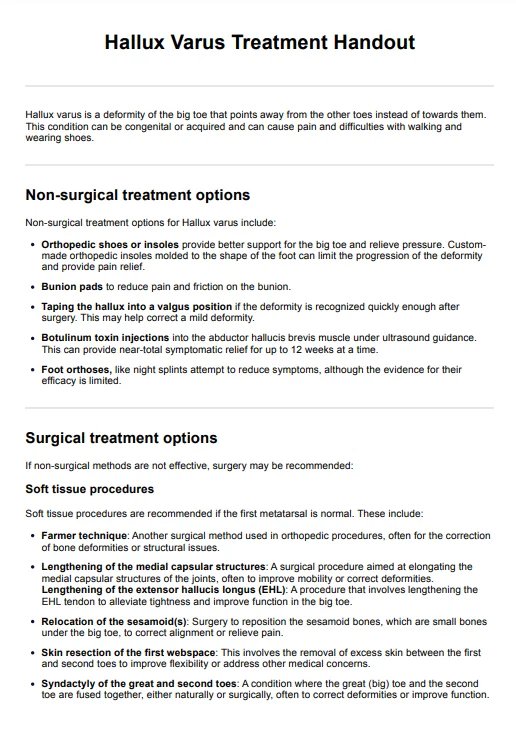
Endocrine Assessment Template
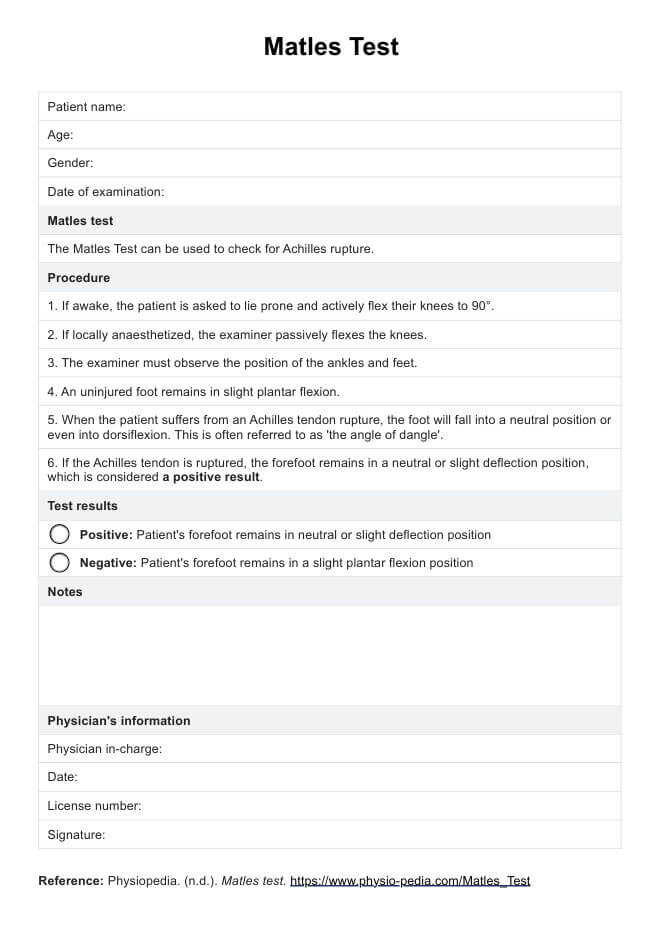
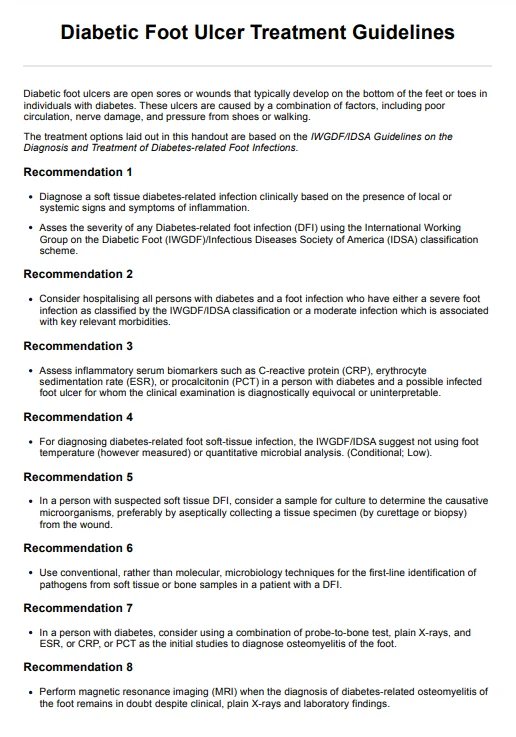
Endocrine Assessment Example
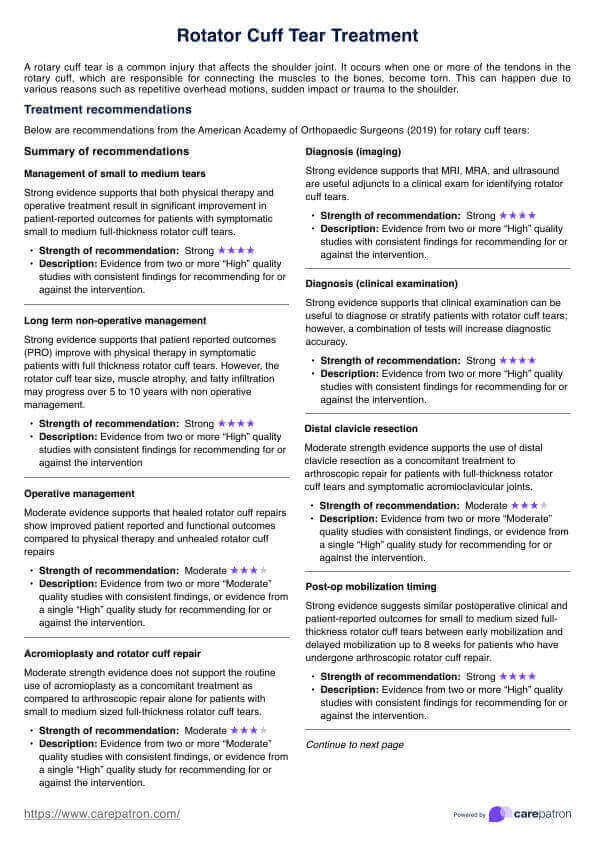
What tests should be expected from an Endocrine Assessment?
Endocrine assessments can involve a variety of diagnostic tests, each aimed at evaluating the function of specific endocrine glands and the hormones they produce. Patients can expect tests such as:
- Thyroid Stimulating Hormone (TSH) and Thyroid Panel: These tests assess thyroid function and are crucial for diagnosing thyroid disease or dysfunction.
- Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH): These are important for evaluating pituitary function and reproductive health issues, such as polycystic ovary syndrome.
- Cortisol tests: Used to diagnose adrenal gland disorders, including adrenal insufficiency and Cushing's syndrome.
- Growth hormone tests: Assess growth hormone levels to diagnose deficiency or excess, which can affect growth and physical development.
- Blood glucose and insulin tests: Essential for diagnosing diabetes mellitus and insulin resistance, conditions related to impaired glucose metabolism.
These tests are part of a comprehensive approach to understanding the patient's endocrine health, guiding the diagnostic process, and developing an effective treatment plan.
Endocrine disorders
Endocrine disorders represent a complex and diverse group of conditions that arise from problems within the body's endocrine system. This system, a network of glands that produce and release hormones, plays a pivotal role in regulating almost every cell, organ, and function in our bodies.
Hormones are chemical messengers that travel through the bloodstream to tissues or organs, working slowly over time to affect many different processes, including growth and development, metabolism, sexual function, reproduction, and mood. When the endocrine glands do not function properly, it can result in an overproduction or underproduction of hormones, leading to endocrine disorders.
Thyroid disorders
Thyroid disorders are among the most common endocrine conditions, affecting the thyroid gland in the neck's front part. The thyroid gland produces thyroid hormones, which regulate metabolism, energy production, and the body's sensitivity to other hormones. Conditions such as hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can drastically affect a person's metabolism and overall energy levels.
Thyroid gland enlargement, known as goiter, and thyroid nodules can also indicate underlying thyroid disease or dysfunction. Treatment often involves hormone replacement therapy, medication to suppress or enhance thyroid function, or surgery in some cases.
Adrenal disorders
The adrenal glands atop the kidneys produce essential hormones such as cortisol, aldosterone, and adrenaline. Adrenal disorders, including adrenal insufficiency (Addison's disease) and Cushing's syndrome, stem from inadequate or excessive production of these hormones.
Adrenal insufficiency can lead to fatigue, muscle weakness, weight loss, and low blood pressure, whereas Cushing's syndrome, often caused by excessive cortisol production, can result in weight gain, high blood pressure, and changes in skin appearance. Treatment varies from hormone replacement for insufficiency to medications or surgery to address hormone overproduction.
Pituitary disorders
The pituitary gland, a small gland at the base of the brain, is often dubbed the "master gland" due to its role in controlling the functions of many other endocrine glands. Pituitary disorders, such as pituitary adenomas (benign tumors) and growth hormone deficiencies, can have widespread effects on the body. These disorders can impact growth, blood pressure, and other aspects of metabolism. Treatment may include medication, hormone replacement therapy, or surgery to remove tumors.
Diabetes mellitus
Diabetes mellitus is a metabolic disorder characterized by high blood sugar levels over a prolonged period. It results from defects in insulin production (Type 1 diabetes), action (Type 2 diabetes), or both. This condition can lead to serious complications if not appropriately managed, including cardiovascular disease, renal failure, and vision problems. Management includes lifestyle modifications, insulin therapy, and medications to control blood glucose levels.
Polycystic Ovary Syndrome (PCOS)
PCOS is a condition that affects women of reproductive age and is characterized by hormonal imbalances, including excess androgen levels and insulin resistance. Women with PCOS may experience irregular menstrual periods, infertility, and polycystic ovaries, along with symptoms like weight gain, acne, and hair thinning. Treatment focuses on managing symptoms and may include lifestyle changes, medication for hormonal balance, and fertility treatments if pregnancy is desired.
Endocrine disorders, due to their hormone-related nature, can have profound effects on an individual's health and quality of life. Early diagnosis and appropriate management are crucial for preventing complications and ensuring effective treatment. This often requires a multidisciplinary approach, including endocrinologists, primary care providers, and specialists in related fields, to address the wide-ranging impacts of these disorders on the body.
Commonly asked questions
Examining the endocrine system involves a combination of clinical evaluation and diagnostic testing. Clinically, healthcare providers assess for physical signs of endocrine dysfunction, such as thyroid gland enlargement, changes in body mass index, or signs of conditions like Cushing's disease. Diagnostic tests, including blood tests for hormones like thyroid stimulating hormone, growth hormone, and cortisol, play a crucial role in confirming the diagnosis.
The assessment of endocrine disorders typically involves a detailed patient history to identify risk factors and symptoms, a physical examination focusing on signs of hormone excess or deficiency, and specific diagnostic tests to measure hormone levels directly. Dynamic tests assessing the endocrine glands' response to stimulation or suppression may also be used for certain conditions.
You should consider seeing an endocrinologist if you have symptoms suggesting an endocrine disorder (such as unexplained weight changes, fatigue, or irregular menstrual cycles) if you've been diagnosed with an endocrine condition and need specialized care (like diabetes mellitus or thyroid disease),, or if your general practitioner recommends consultation for complex hormonal issues.

.jpg)