That depends. This scale comes with several activities that need to be done to score the patient, so it may take 15 minutes to an hour.
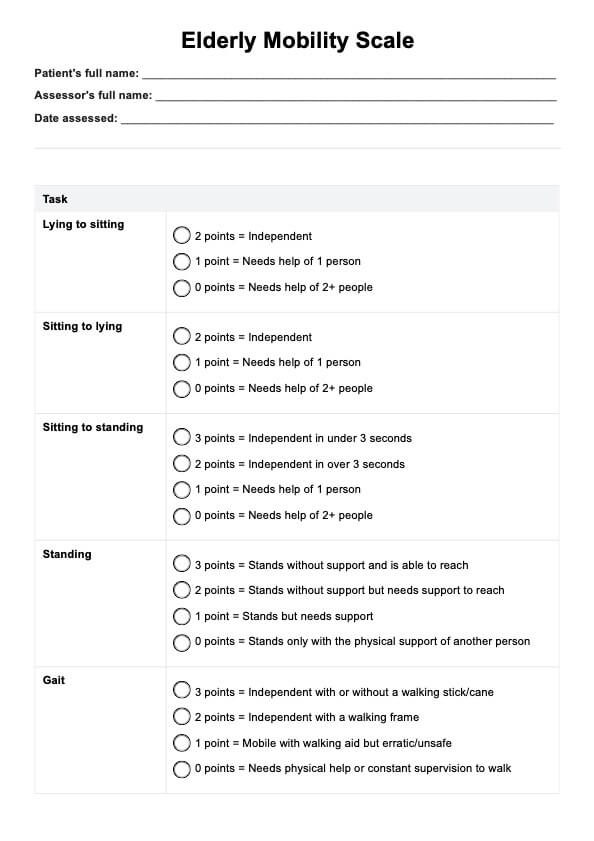
Elderly Mobility Scale
If you are treating a supposedly frail elderly patient, you can gauge them using the Elderly Mobility Scale to assess their mobility. Learn more about this scale with this guide!
Elderly Mobility Scale Template
Commonly asked questions
Yes. These activities involve a person’s mobility, and since the primary population for this scale is elderly people, they are at risk of losing their balance. That’s why you and your assistants should help support these patients while performing the activities so they don’t get hurt.
Of course, if you ever conduct a house call, you can definitely administer this in a home setting, so long as you have the needed equipment.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











