This will depend on the patient you’re assessing, but it’s possible to accomplish the assessment within 20 minutes. Don’t be surprised if it takes longer, though.
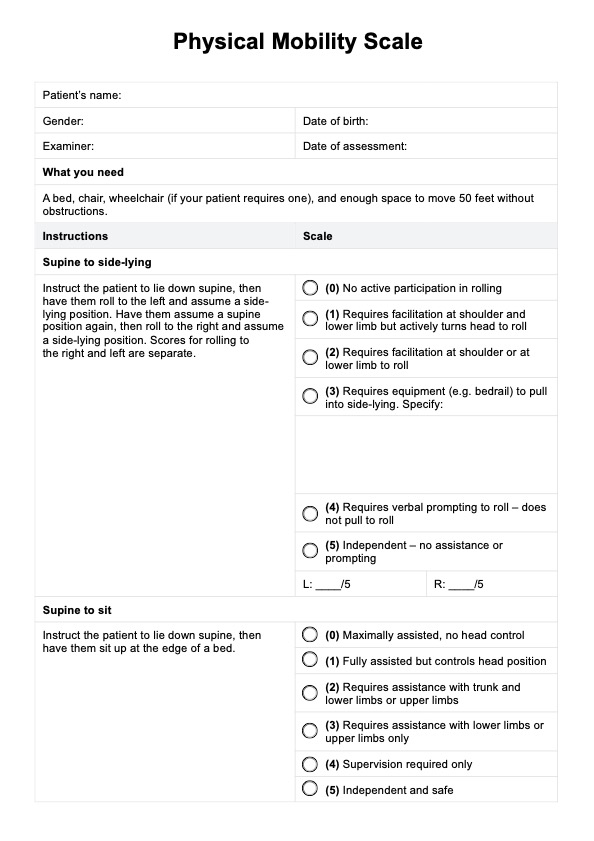
Physical Mobility Scale
Learn about the Physical Mobility Scale and use our template to assess older adults and their ability to perform certain movements!
Use Template
Physical Mobility Scale Template
Commonly asked questions
Yes. For consistency, it would be best to conduct additional balance tests.
It would be best to conduct this every time a patient returns for a check-up or if it’s time for a scheduled house call. This isn’t a one-time, big-time assessment. As we mentioned earlier, this is an effective monitoring tool, so using it routinely will ensure you are on top of your geriatric patient’s mobility status.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











