It can be accomplished within five minutes.
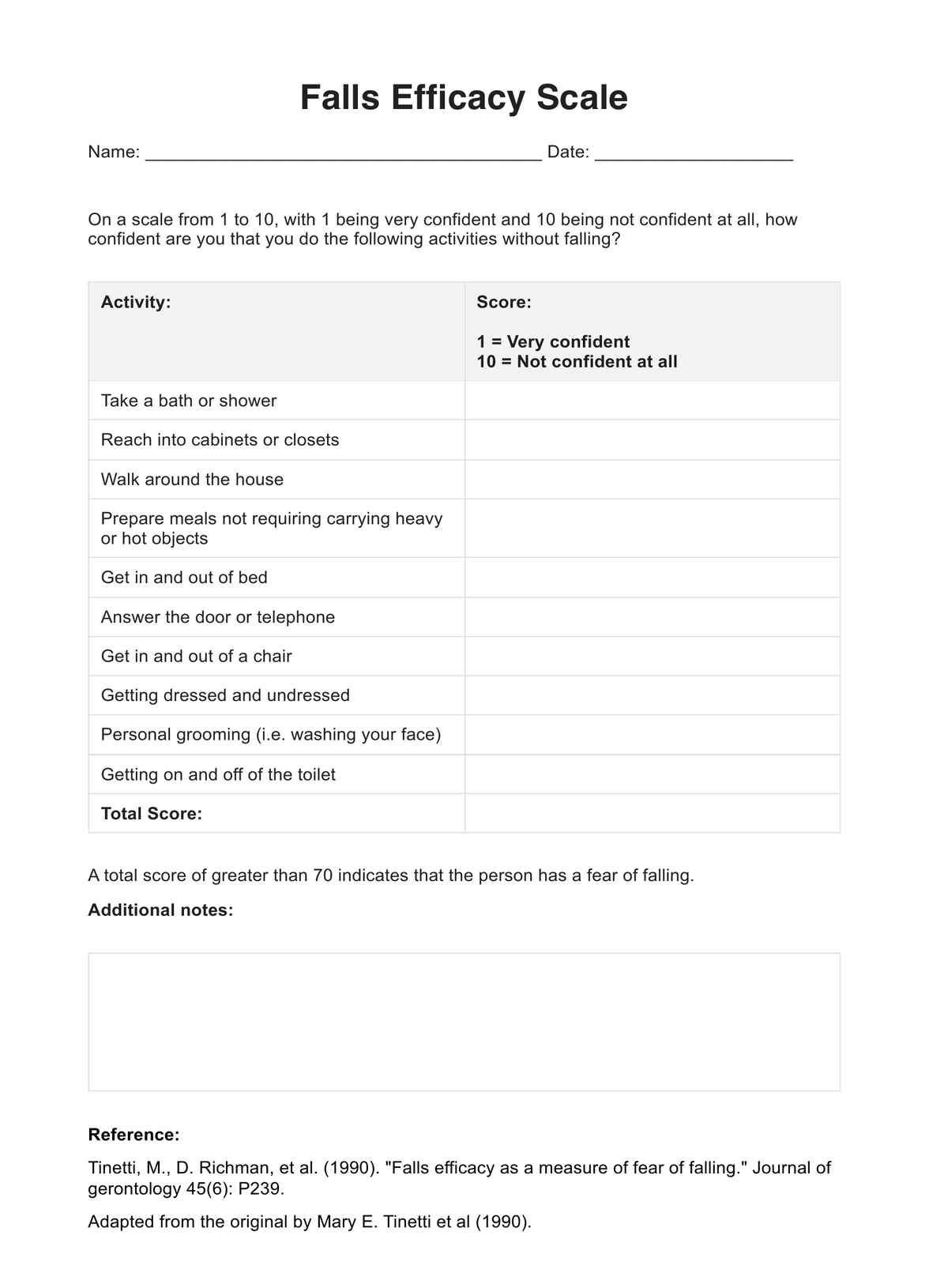
Use the Falls Efficacy Scale to gauge how afraid your patient is of falling while doing activities of daily living.
It can be accomplished within five minutes.
You can conduct the scale in an interview format. Just explain what they need to do, then have them say what their self-ratings are. You can jot them down on the sheet. If you conduct it like an interview, you can have them expound on their self-ratings and record them in the comments box.
Geriatricians, physical therapists, neurologists, and adjacent healthcare professionals can use this scale.
EHR and practice management software
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments