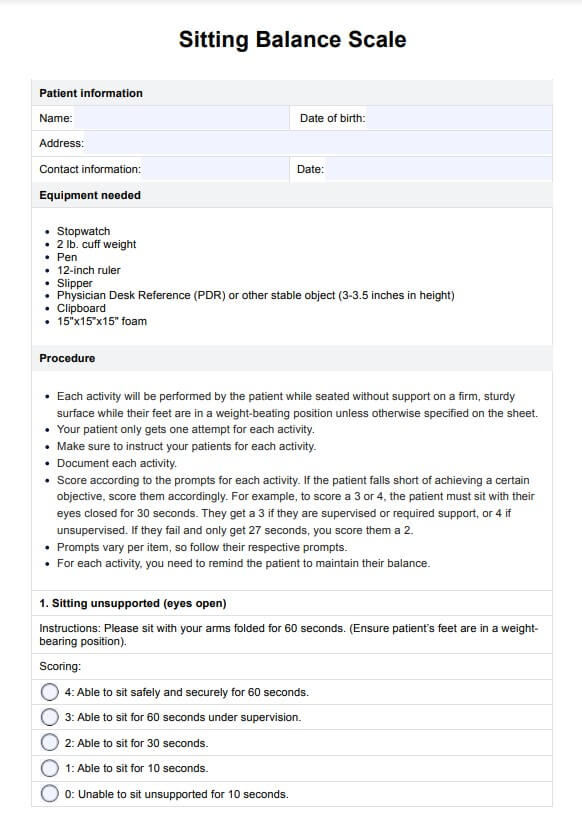
The patient performs tasks like sitting unsupported, reaching forward, and picking up objects. Each task is scored on a 5-point scale, with 0 representing the lowest ability and 4 indicating that the patient can successfully complete tasks confidently in a sitting position.
Sitting Balance Scale
Use the Sitting Balance Scale to gauge the capability of mostly non-ambulatory patients to balance themselves while sitting, standing, and moving.
Sitting Balance Scale Template
Commonly asked questions
The Sitting Balance Scale is considered a reliable and valid tool for assessing an individual's seated balance. It effectively measures balance abilities and can predict fall risk. It is correlated with other assessments, such as the Berg Balance Scale and the Lower Extremity Functional Scale. This makes it a valuable instrument for clinicians to assess and monitor balance interventions over time.
The test typically takes about 15-20 minutes, depending on the patient’s ability to complete tasks successfully.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











