Peripheral Vascular Disease (PVD) refers to disorders affecting blood vessels outside the heart and brain. It primarily involves narrowing peripheral arteries (most commonly in the legs) due to plaque buildup. This leads to reduced blood flow, causing symptoms such as leg pain, numbness, and, in severe cases, ulcers or gangrene.
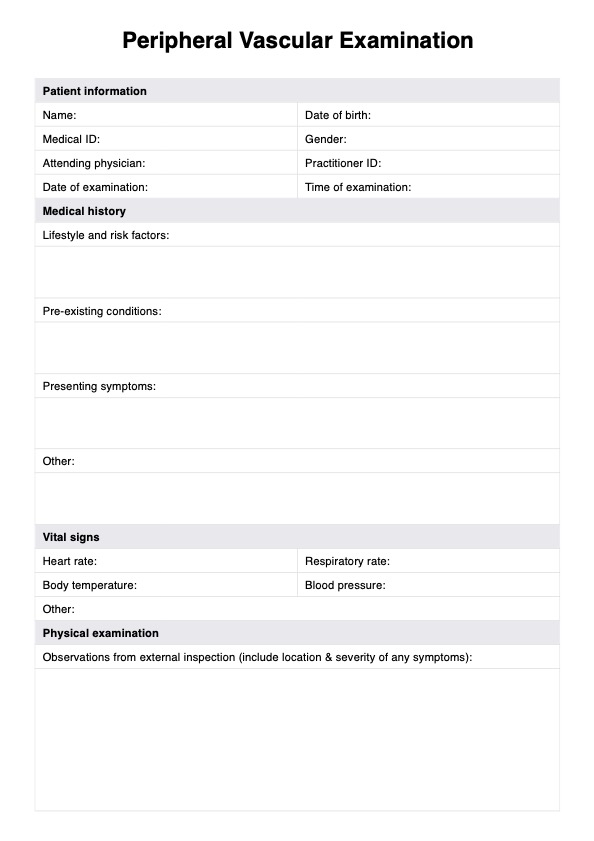
Peripheral Vascular Examination
Explore our comprehensive Peripheral Vascular Examination guide for detailed assessment and documentation of vascular health, including key tests and findings.
Peripheral Vascular Examination Template
Commonly asked questions
The primary cause of PVD is atherosclerosis, where fatty deposits build up in the arterial walls and restrict blood flow. Other risk factors include smoking, diabetes, obesity, high blood pressure, high cholesterol, aging (especially over age 50), and a family history of vascular or heart diseases.
Symptoms vary depending on the part of the vascular system affected but typically are the result of reduced blood flow to the limbs. Edema (increased swelling), numbness, coldness, and weakness, claudication, and reduced peripheral pulses in the bilateral lower extremities are common. Other symptoms may include claudication, limb hair loss, erectile dysfunction, sores that won't heal, shiny skin, and change in skin color (paleness or cyanosis).
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











