The primary function of the musculoskeletal system is to provide the body with structural support surrounding tissue, enable movement through muscle contraction, and protect vital internal organs.
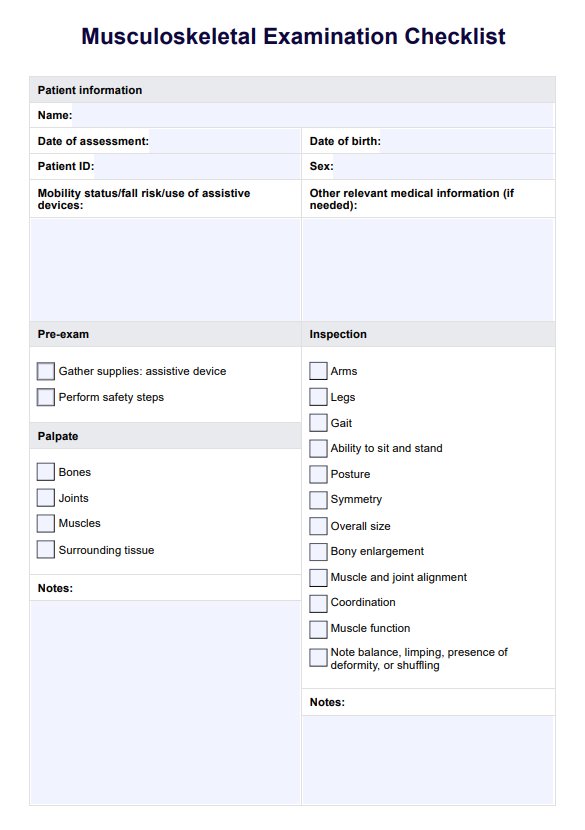
Musculoskeletal Examination Checklist
Ensure you don't miss a step when conducting a musculoskeletal assessment by following a guide like our free Musculoskeletal Examination Checklist.
Musculoskeletal Examination Checklist Template
Commonly asked questions
While not all musculoskeletal problems can be prevented, maintaining a healthy lifestyle with regular exercise, a balanced diet rich in calcium and vitamin D, proper posture, and using ergonomic tools can significantly reduce the risk of developing many musculoskeletal conditions.
Healthcare providers assess muscle strength during a musculoskeletal assessment by asking patients to perform various movements against resistance. This helps evaluate the function and strength of symmetrical muscle groups and identify any discrepancies in evaluating muscle strength that might indicate underlying conditions.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











