Diagnostic criteria identify and diagnose a disease in individual patients, while classification criteria categorize conditions for research and study purposes.
Osteoarthritis Diagnosis Criteria
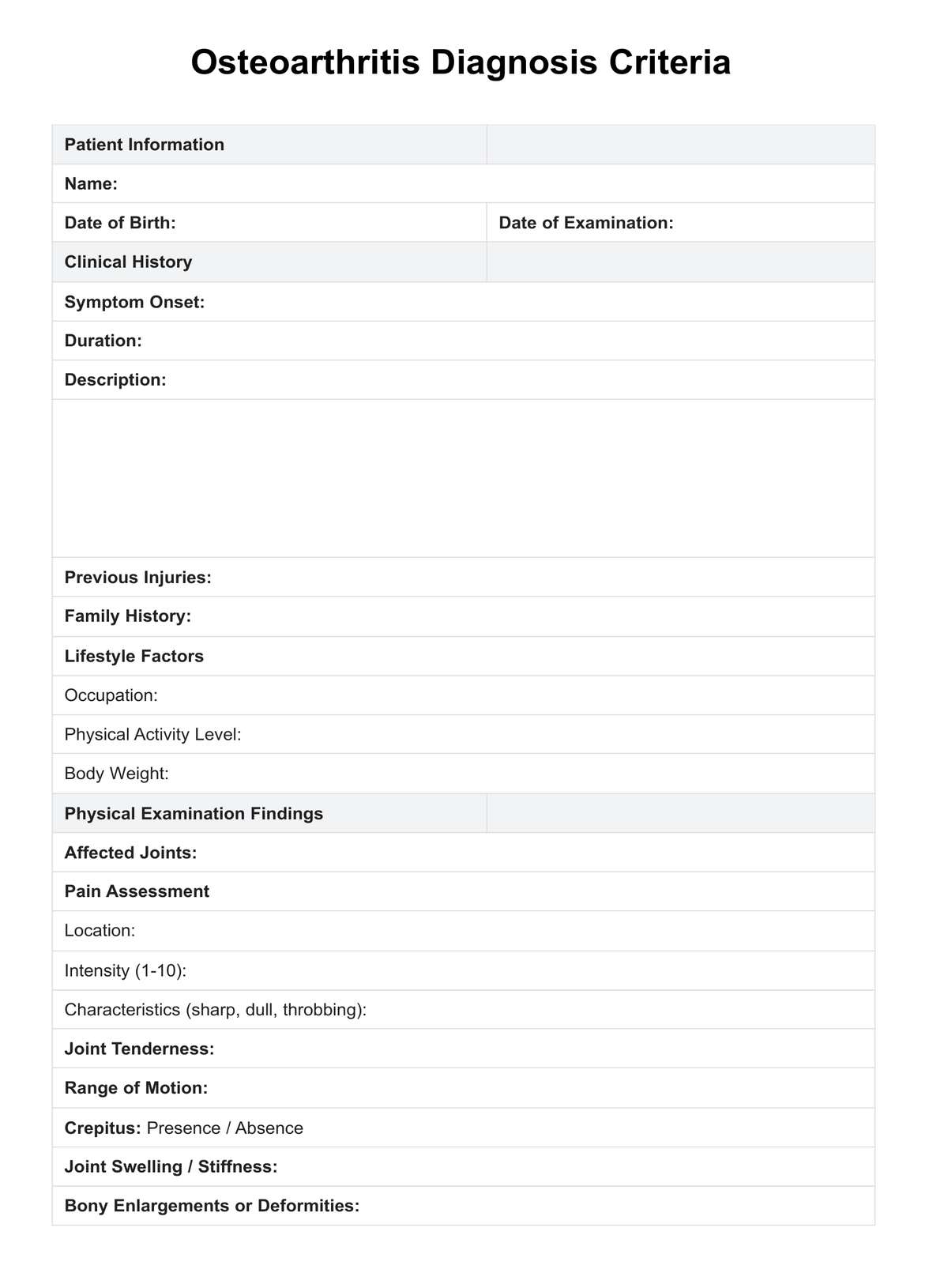
Understand the signs, causes, and effective criteria for diagnosis. Download our free PDF example for a detailed understanding.
Osteoarthritis Diagnosis Criteria Template
Commonly asked questions
Arthritis is a broad term for conditions causing joint pain and inflammation. Osteoarthritis is a specific type of arthritis characterized by the wear and tear of joint cartilage.
Osteoarthritis diagnosis involves a physical exam, patient history review, and imaging tests like X-rays to detect joint changes. Blood tests may exclude other conditions. These steps confirm the diagnosis, guiding the treatment plan to manage symptoms and improve life quality.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











