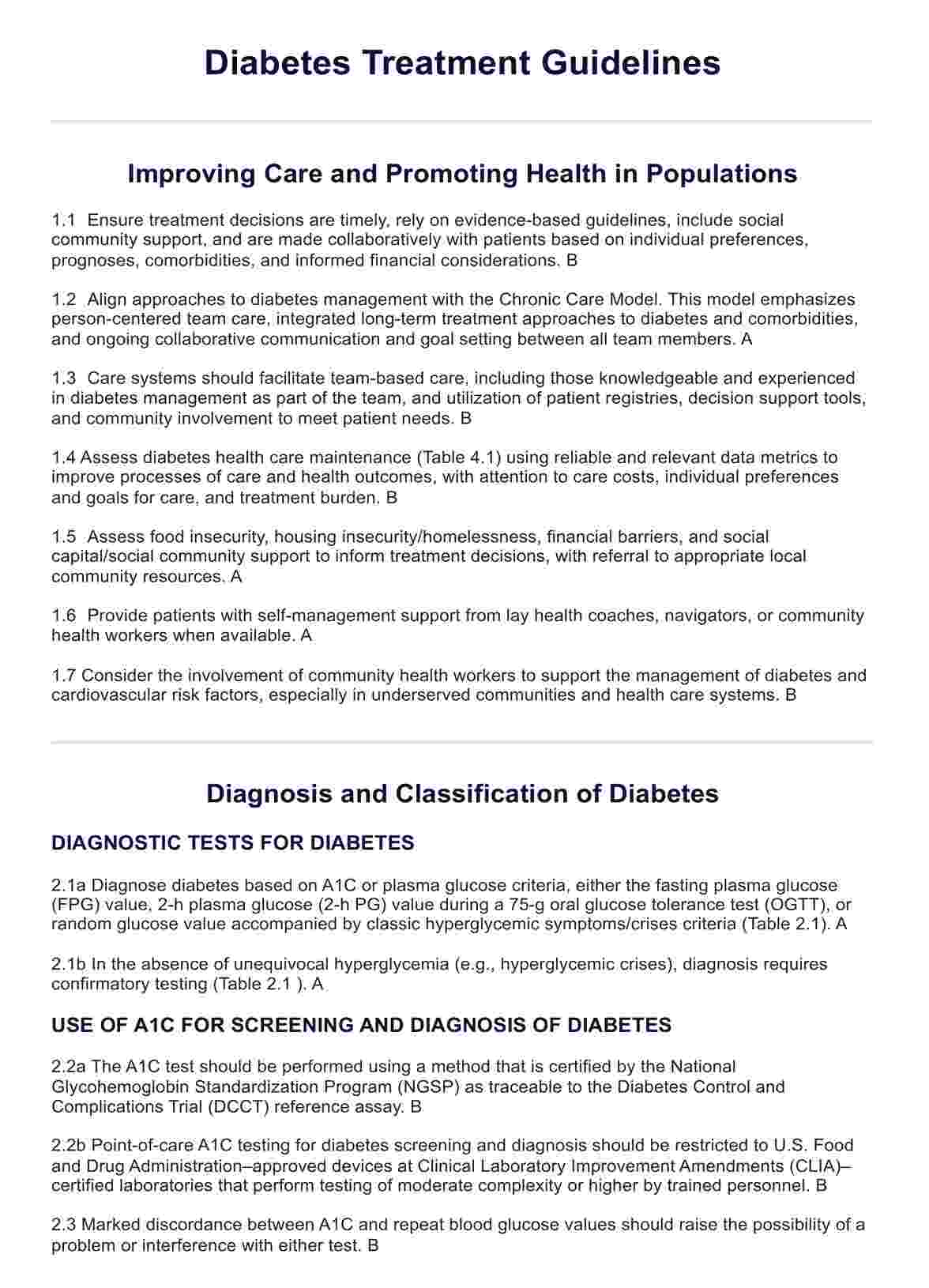
These guidelines serve as a roadmap for healthcare providers, offering standardized approaches to diagnosing, treating, and managing diabetes. They help ensure consistency, quality of care, and improved patient outcomes.
Diabetes Treatment Guidelines
Explore comprehensive Diabetes Treatment Guidelines for effective management and improved health outcomes.
Use Template
Diabetes Treatment Guidelines Template
Commonly asked questions
Diabetes Treatment Guidelines are typically developed by expert panels comprising healthcare professionals, researchers, and other stakeholders. Organizations like the ADA regularly review scientific evidence to update and refine these guidelines.
Diabetes Treatment Guidelines cover various topics, including screening and diagnosis, glycemic control targets, medication management, lifestyle interventions, and strategies for preventing diabetes-related complications.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











