To create a comprehensive nursing care plan for fluid volume management, customize the plan from the scaffolding provided by Carepatron and cater to the patient's needs through the critical aspects of assessment, diagnosis, intervention, and evaluation.
Fluid Volume Deficit Nursing Care Plan
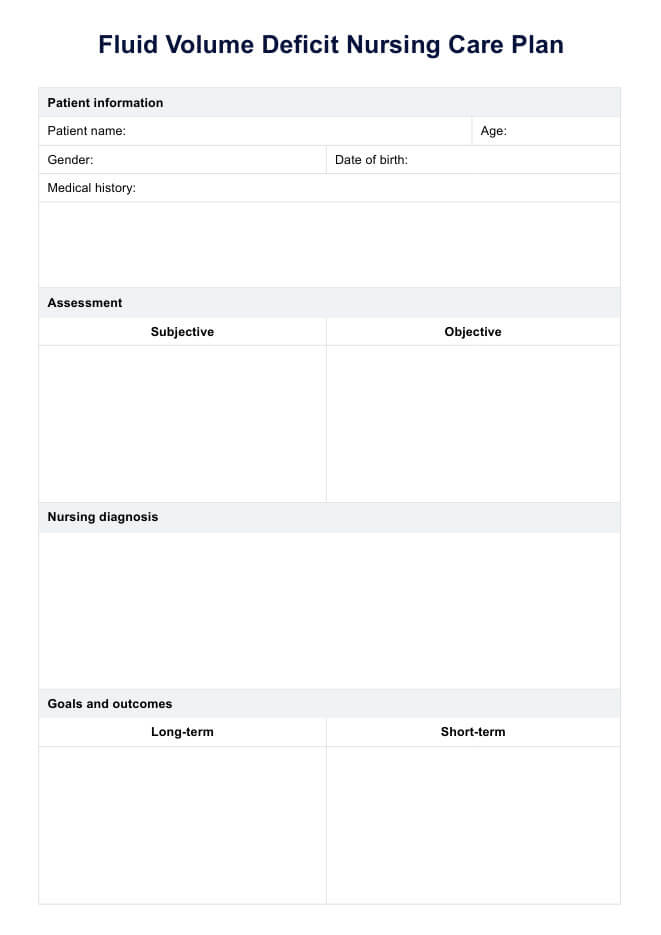
Create a fluid volume deficit nursing care plan with clear steps to assess, monitor, and manage hydration, ensuring patient safety and recovery.
Use Template
Fluid Volume Deficit Nursing Care Plan Template
Commonly asked questions
These valuable plan templates can be used at any point of the treatment journey for a patient with fluid volume deficit to track, monitor, and plan all interventions by healthcare professionals and the patient themselves.
Fluid deficit nursing care plan templates plan efficient and confident care delivery. They are designed to be customized and meet the individual patient's needs.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











