Migraines typically present with moderate to severe headaches, often accompanied by nausea, vomiting, and sensitivity to light and sound. Some individuals may experience an aura—transient neurological symptoms—before the onset of the headache.
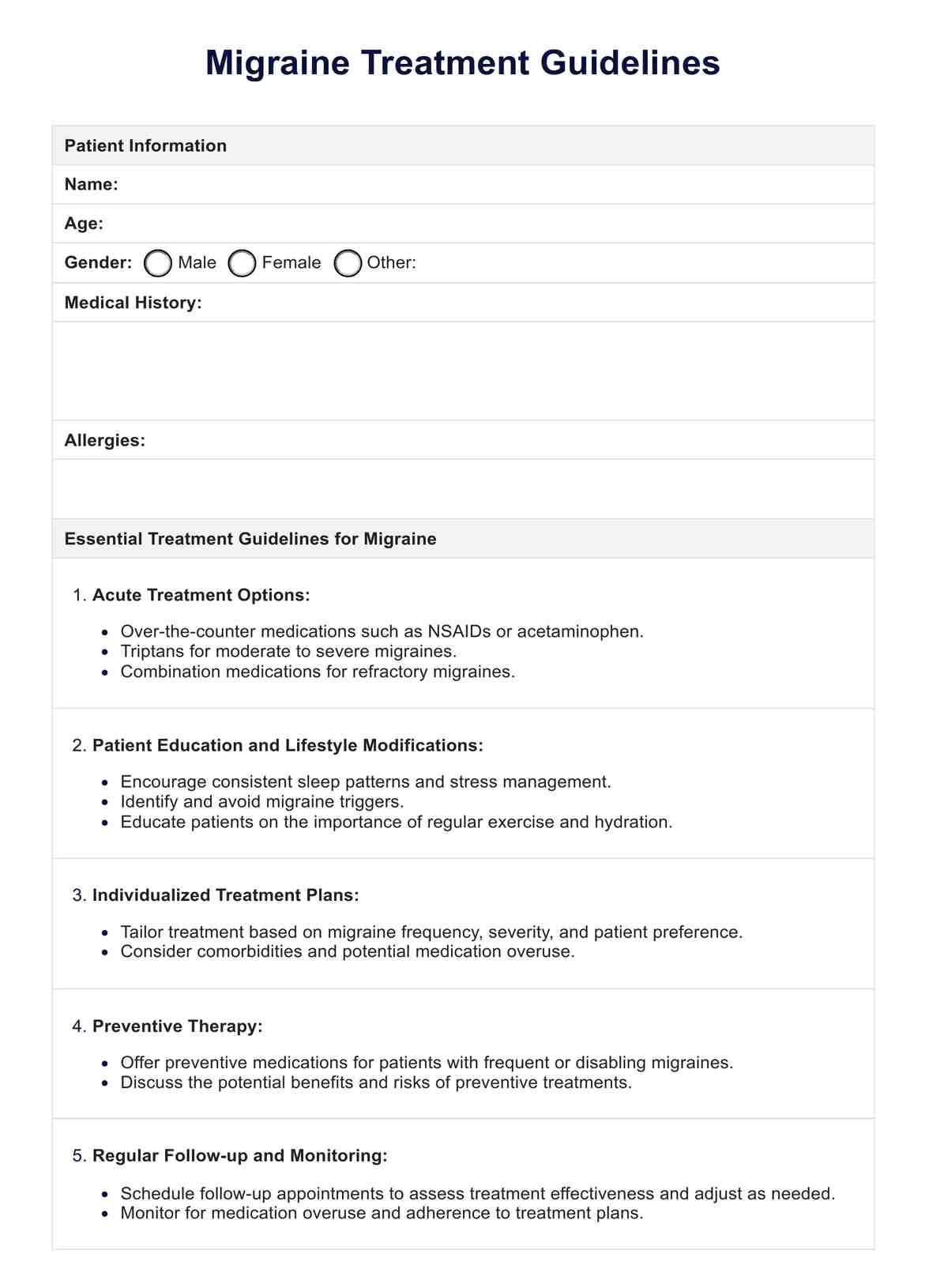
Migraine Treatment Guidelines
Learn effective Migraine Treatment Guidelines to relieve debilitating headaches and improve your quality of life.
Use Template
Migraine Treatment Guidelines Template
Commonly asked questions
Migraines are neurological conditions characterized by recurrent, often disabling headaches, whereas tension headaches are generally milder and result from muscle tension or stress.
Diagnosis of migraines is primarily based on clinical evaluation, including a thorough assessment of symptoms, medical history, and physical examination. Additional tests, such as imaging studies, may be conducted to rule out other potential causes of headaches.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











