Qualified healthcare professionals, such as physiotherapists, occupational therapists, and nurses trained in stroke rehabilitation, are typically eligible to perform the PASS Assessment.
PASS Assessment
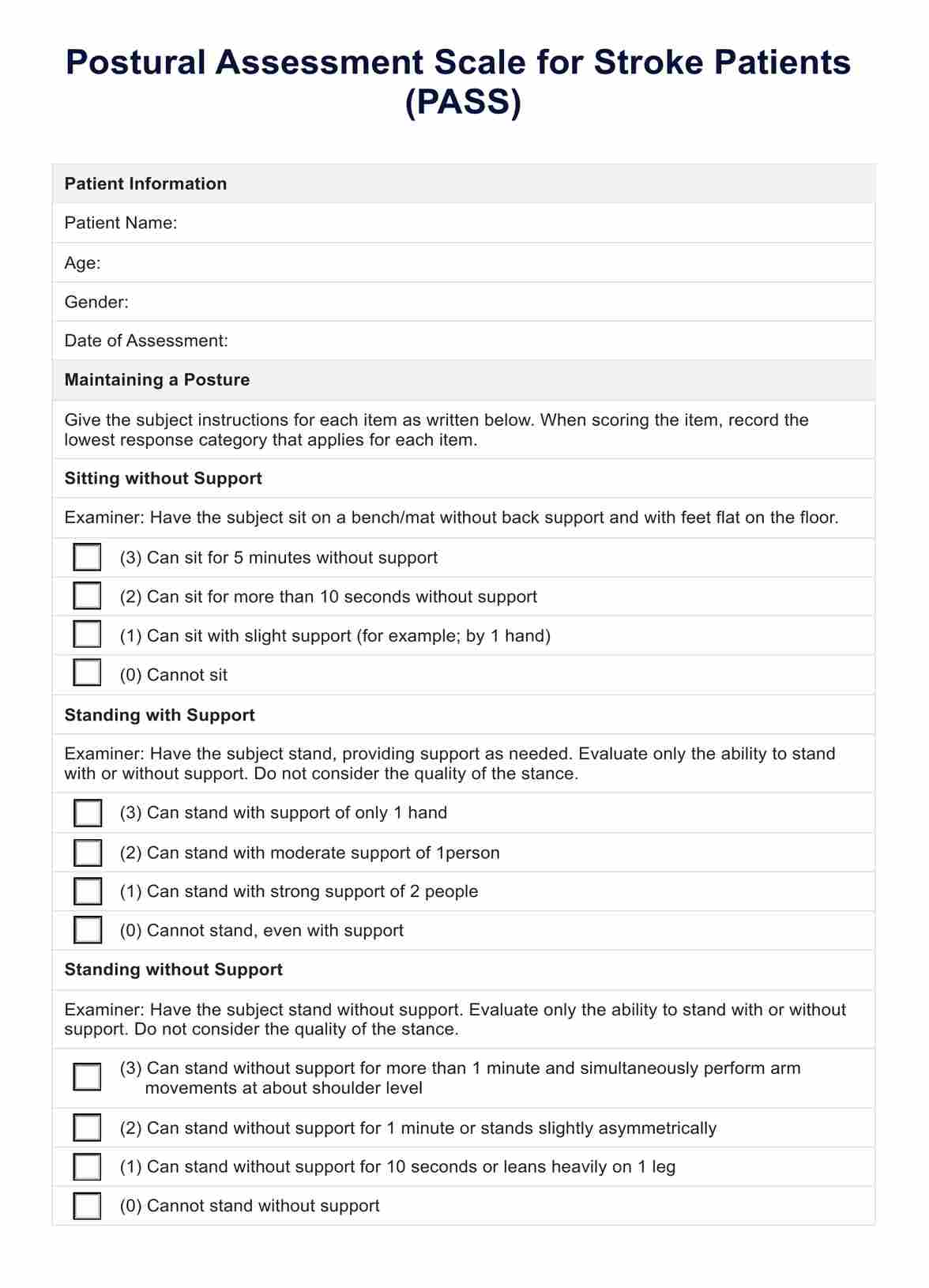
Explore the use of a specialized test to assess postural control among stroke patients to craft a more targeted rehabilitation plan.
Use Template
PASS Assessment Template
Commonly asked questions
It measures a stroke patient's ability to perform various postural tasks, including lying, sitting, standing, and changing positions, with each position graded on a scale.
The frequency of assessment depends on the clinical setting and the patient's rate of recovery. It can be used as a baseline measurement and periodically reassessed to monitor progress.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











