The blood test assesses the presence of lupus anticoagulant, an antibody associated with an increased risk of abnormal blood clotting.
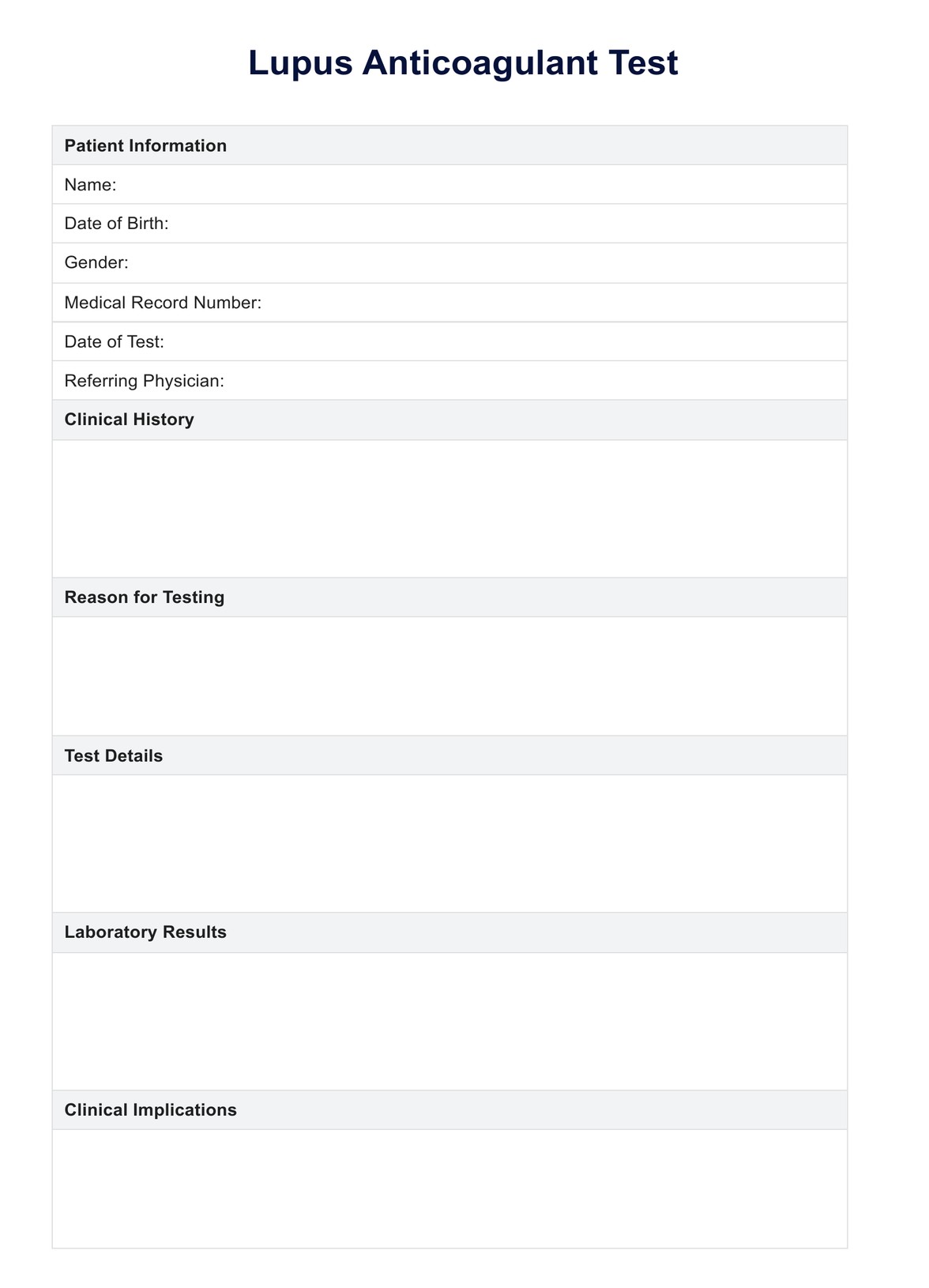
Lupus Anticoagulant Test
Unlock the mysteries of the Lupus Anticoagulant Test with our comprehensive guide—your go-to resource for understanding, testing, and implications.
Use Template
Lupus Anticoagulant Test Template
Commonly asked questions
The test is performed to diagnose or monitor conditions such as antiphospholipid syndrome, recurrent thrombosis, and unexplained pregnancy complications.
The test typically involves measuring clotting times, such as activated partial thromboplastin time (aPTT) or dilute Russell Viper Venom Time (dRVVT), before and after adding patient plasma.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











