An Integrated Treatment Plan is a comprehensive, patient-centered approach that addresses both mental health and substance use disorders simultaneously. It ensures coordinated care by involving a multidisciplinary team to tailor interventions to the individual’s specific needs and goals. This dynamic plan evolves to reflect the patient’s progress and changing circumstances.
Integrated Treatment Plan
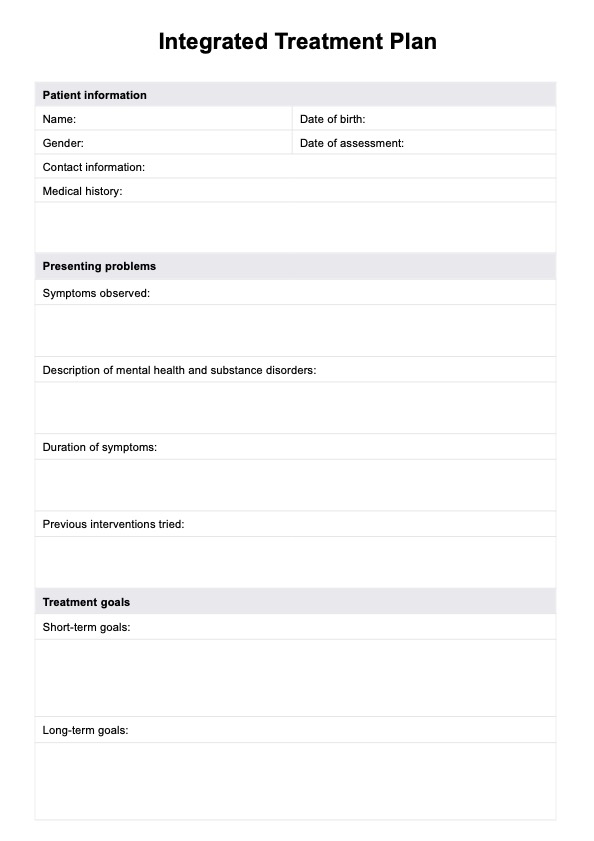
Download Carepatron's free Integrated Treatment Plan PDF template to help you create effective treatment plans for patients.
Integrated Treatment Plan Template
Commonly asked questions
Effective integrated treatment includes evidence-based practices such as cognitive-behavioral therapy, medication management, and motivational interviewing. It emphasizes a holistic approach, addressing physical health, mental health, and social factors like housing and employment. Key elements also include continuous care, family involvement, and strategies for relapse prevention.
The integrated behavior treatment model is a unified approach designed to address co-occurring disorders by simultaneously treating substance use disorders and mental health symptoms. It integrates interventions to ensure consistency and minimize fragmented care, creating a more effective treatment experience. This model emphasizes patient-centered care, fostering collaboration, adaptability, and long-term recovery for individuals managing complex challenges.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











