A Musculoskeletal Nursing Assessment includes evaluating muscle strength, joint function, and range of motion, alongside identifying pain, swelling, or deformities. It also incorporates inspection, palpation, and strength testing using tools like the muscle strength testing scale for comprehensive evaluation.
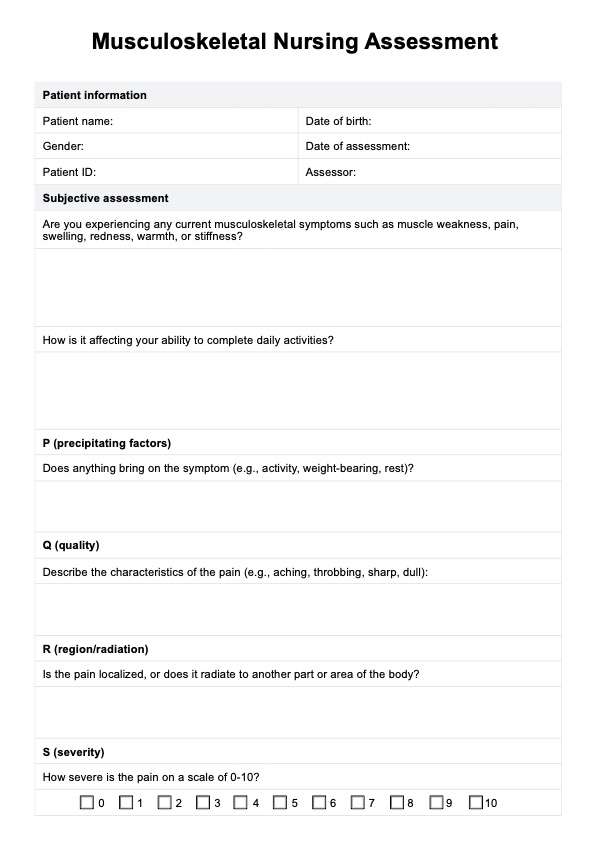
Musculoskeletal Nursing Assessment
Learn about the important aspects and key components when assessing patients through Carepatron's Musculoskeletal Nursing Assessment PDF.
Musculoskeletal Nursing Assessment Template
Commonly asked questions
Nurses use observation, palpation, and functional tests to evaluate the musculoskeletal system, observe the condition of joints, inspect muscles, and other relevant aspects. Tools such as the trace muscle contraction method or a fall risk scale may also be used to assess conditions like weakness or instability.
During inspection, nurses assess posture, symmetry, and alignment of muscles and joints while noting swelling, redness, or deformities. The evaluation also includes checking for abnormalities in motion or visible signs of injury, like a strained lateral collateral ligament.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











