When documenting a normal abdominal assessment, ensure to note the absence of pain or tenderness, a lack of visible lesions or distension, and normal bowel sounds. Record each quadrant systematically to confirm that the patient's abdomen is soft and non-tender upon light palpation.
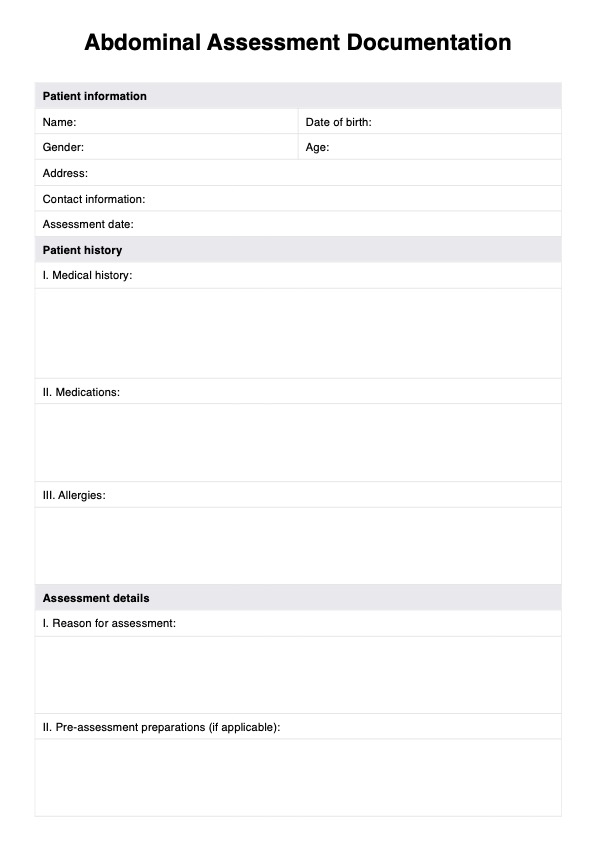
Abdominal Assessment Documentation
Properly document abdominal assessment findings with our free Abdominal Assessment Documentation template. Access it for free today!
Abdominal Assessment Documentation Template
Commonly asked questions
A focused gastrointestinal and genitourinary assessment gathers information on symptoms, digestive or nutritional issues, medical or family history, and current treatments for GI and GU conditions.
Normal findings in an abdominal assessment include a flat or rounded abdomen without visible scars or lesions, normoactive bowel sounds occurring at regular intervals, and no tenderness or pain upon palpation. Additionally, the abdomen should not show signs of swelling, and organs like the liver and spleen should not be palpable under normal conditions.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











