Mental health and medical history should be included in the Subjective section. This is where you document the patient's words about their past conditions and concerns.
Soap Chart
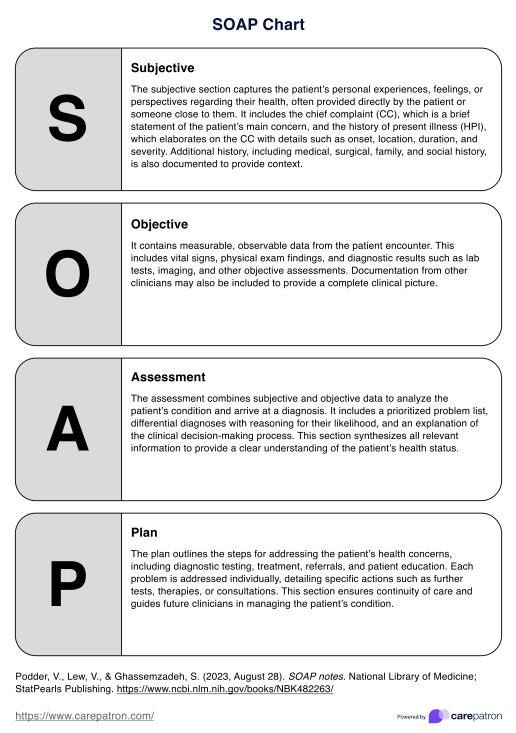
Write SOAP notes with ease! Access this quick-reference SOAP Chart to know what to include and streamline your patient documentation efficiently.
Use Template
Soap Chart Template
Commonly asked questions
Medications and allergies can be documented in either the Subjective or Objective sections. Be sure to include essential details for each medication, such as its name, dosage, route, and frequency.
SOAP stands for Subjective, Objective, Assessment, and Plan. It’s a format healthcare professionals use to document patient information, ensuring clear and organized notes.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











