A SOAP note in nutrition is a structured documentation format used by dietitians and nutritionists to record patient encounters, assessments, and treatment plans. It follows the SOAP framework: subjective (patient-reported information like dietary habits, symptoms, and medical history), objective (measurable data such as weight, lab results, and food intake records), assessment (analysis of nutritional issues or diagnoses), and plan (interventions, dietary recommendations, and follow-up plans).
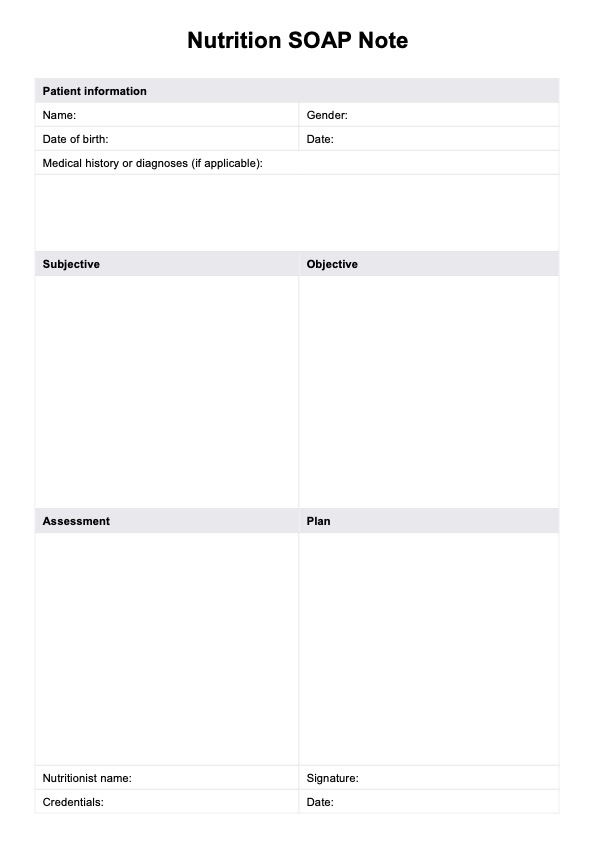
Nutrition SOAP Note
Download our free Nutrition SOAP Notes template now to optimize your nutrition practice with structured documentation to improve patient care.
Nutrition SOAP Note Template
Commonly asked questions
An example of a Nutrition SOAP Note could include: Subjective: The patient reports poor appetite and a 4 kg weight loss over two months; Objective: The BMI is 18.5; lab results show low albumin levels. Assessment: The patient is at risk for malnutrition due to inadequate intake and weight loss. Plan: Recommend small, frequent meals with high-protein snacks; prescribe oral nutritional supplements; schedule follow-up in two weeks to monitor progress.
To document nutritional status effectively, gather subjective data (e.g., patient history, appetite, and food preferences) and objective data (e.g., weight, BMI, and lab results). Assess the findings to identify nutritional risks or deficiencies and create a plan with specific dietary adjustments or supplementation interventions. Ensure documentation is clear, systematic, and includes measurable outcomes to facilitate follow-up and interdisciplinary communication.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











