Considering the number of things you must do; it’ll take at least an hour.
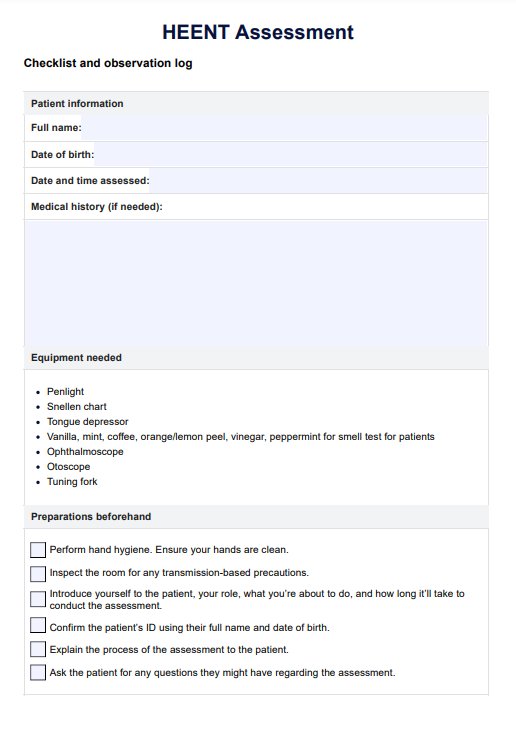
HEENT Assessment
The HEENT Assessment is a comprehensive examination conducted during routine physical examinations. Learn more about it through this guide.
Use Template
HEENT Assessment Template
Commonly asked questions
The HEENT Assessment allows professionals to check for infections, lesions, nasal polyps, signs of oral cancer, and more abnormalities.
The assessment can cause discomfort since the professional will be palpating certain parts of the head and neck. The professional should inform patients about such things before even beginning the assessment so they know what they’re up for.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











