A swallowing test typically involves the patient consuming various food and liquid consistencies while a healthcare professional observes the swallowing process. This assessment may use tools like fiberoptic endoscopic evaluation or modified barium swallow to provide detailed insights into the oral, pharyngeal, and esophageal phases of swallowing.
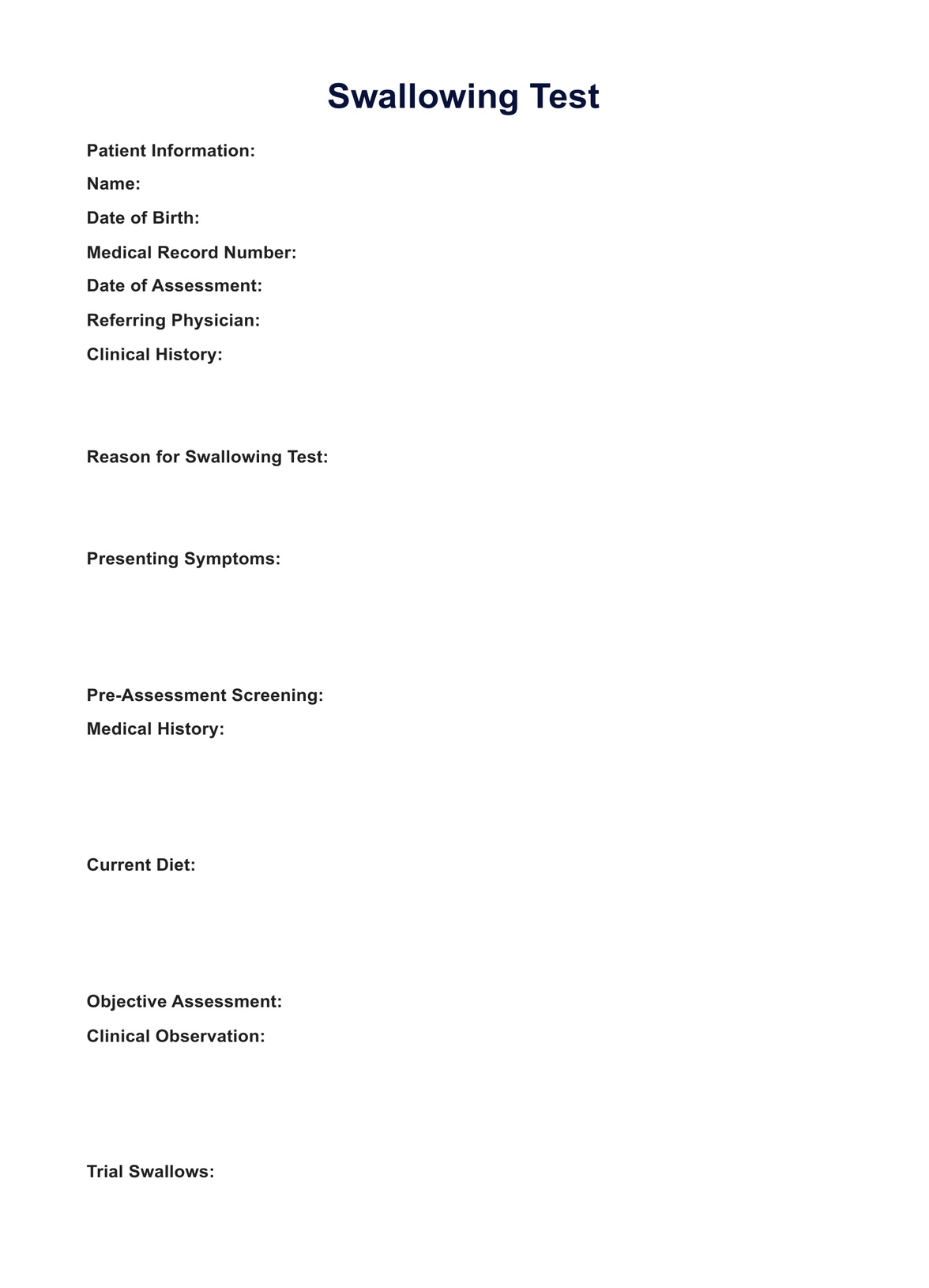
Swallowing Test
Learn about the Swallowing Test and its importance in diagnosing swallowing disorders, and get access to a free PDF download.
Swallowing Test Template
Commonly asked questions
Failing a swallow test indicates potential difficulties or abnormalities in swallowing function. The following steps may involve further diagnostic tests, consultation with specialists, and implementing targeted interventions, such as modified diets or swallowing therapy, to address the identified issues.
Diagnostic tests for difficulty swallowing may include a modified barium swallow (MBS), fiberoptic endoscopic evaluation of swallowing (FEES), or a clinical swallowing examination. These tests help identify the underlying causes of swallowing difficulties, allowing healthcare professionals to develop tailored treatment plans.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











