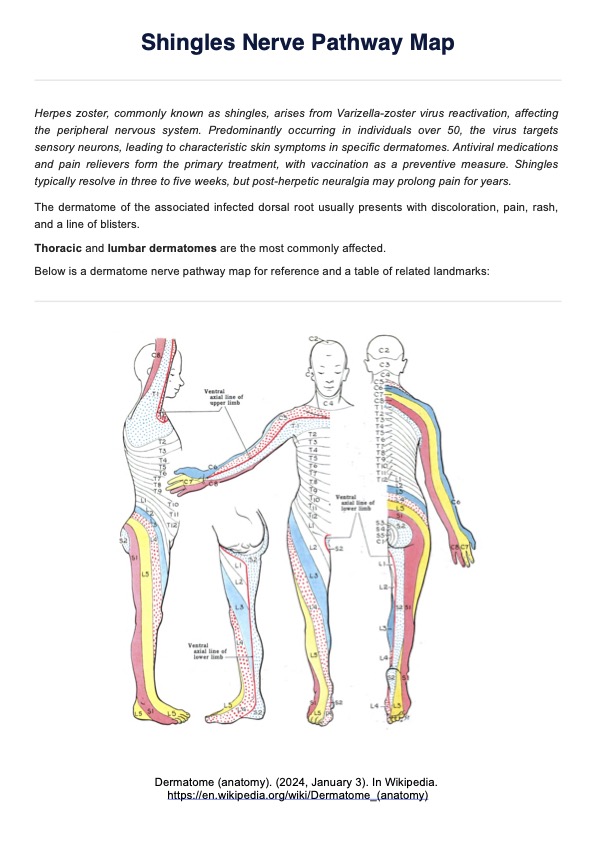
The classic pattern runs along a nerve root from the spine to the rib and all the way to the front of the chest.
Shingles Nerve Pathways Map
Looking for a Shingles Nerve Pathways Map? Get the gist of shingles and its pathways by downloading our handout.
Use Template
Shingles Nerve Pathways Map Template
Commonly asked questions
In rare cases, it may.
The map correlates the distribution of the shingles rash with specific spinal nerves, allowing clinicians to accurately diagnose affected areas and manage nerve pain effectively.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











