The easiest way to get a return-to-work note is often through a walk-in visit to an urgent care clinic or by scheduling a virtual appointment via a telemedicine service, as these options generally offer faster service than a primary care physician. Before your visit, you should check with your employer for any specific requirements for the note and bring your ID and insurance, then clearly explain to the provider that you need documentation clearing you to resume your work duties, along with any necessary restrictions or accommodations.
Return To Work Doctors Note
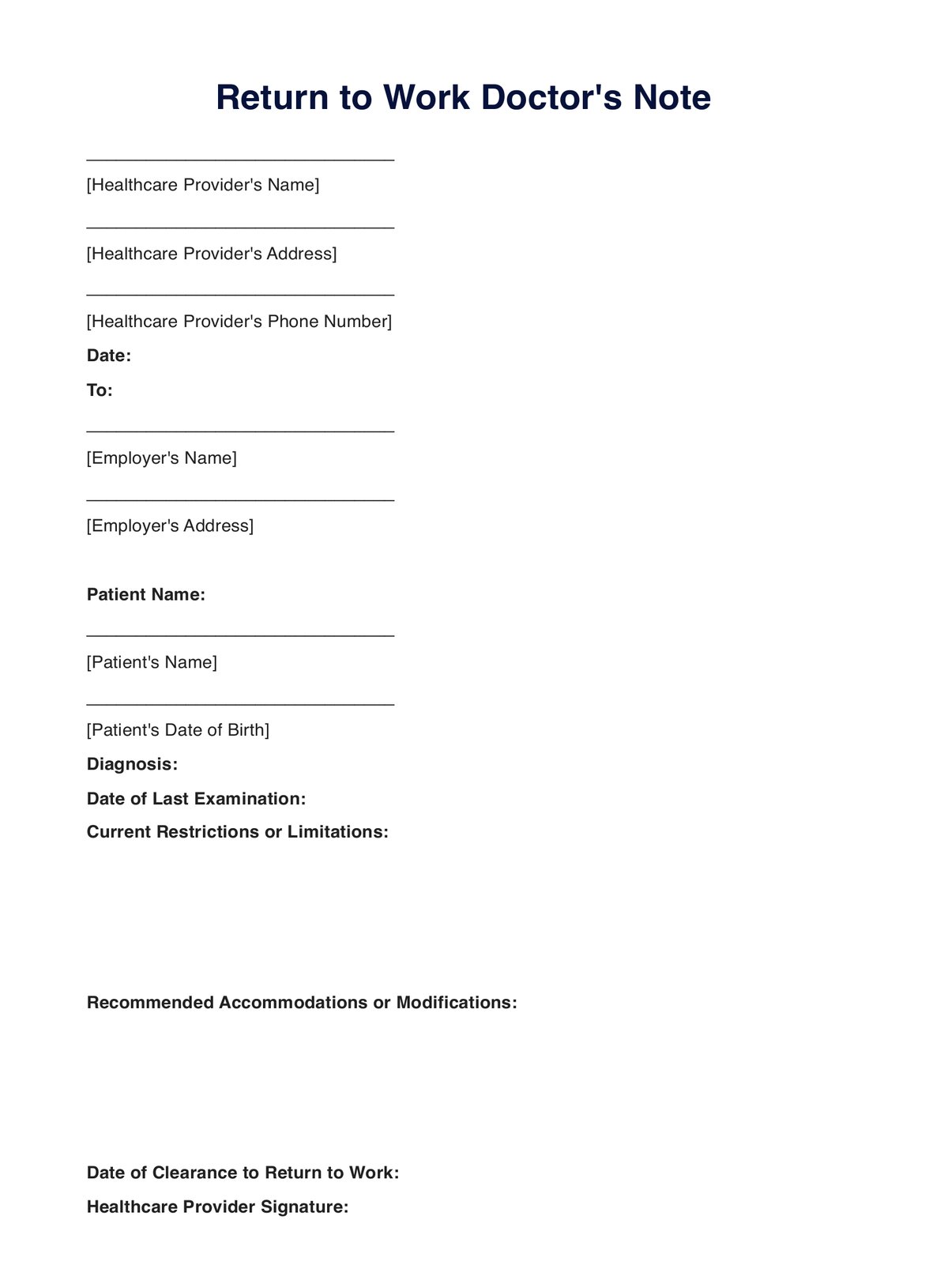
Download our return to work doctor's note template to provide official medical documentation for patients resuming job duties.
Return To Work Doctors Note Template
Commonly asked questions
A return to work form should typically include your name, job title, the first and last days of your absence, the total duration, the reason for the absence, and confirmation of any necessary medical certification (like a "fit note" from your doctor). Critically, it should also summarize any discussions about workplace adjustments or accommodations needed to support your safe return and be signed by both you and your manager.
An employer may refuse a doctor's note if it appears fraudulent, is vague or incomplete, or does not meet the specific requirements of the company's policy (like being from an unapproved provider). If your valid note is rejected, you should first seek clarification from your HR department in writing; if the refusal seems arbitrary, discriminatory, or violates federal laws like the Family and Medical Leave Act (FMLA) or the Americans with Disabilities Act (ADA), you may need to file a complaint with the Department of Labor or the Equal Employment Opportunity Commission (EEOC), or consult with an employment lawyer.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











