A Retinal Detachment Test is an eye examination procedure used to identify whether there is damage at the site of the retina, specifically if the retina has become detached from the blood vessels.
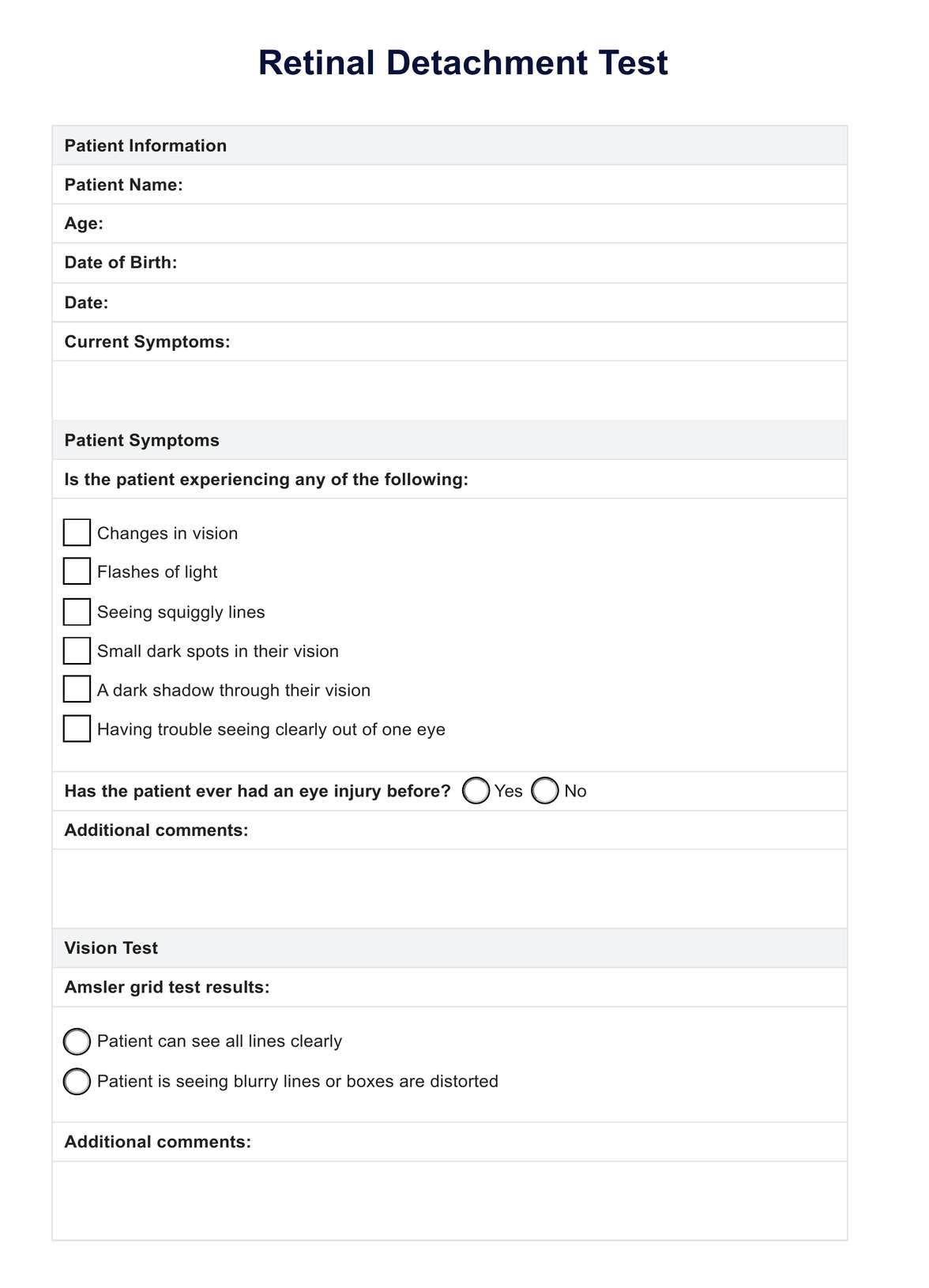
Retinal Detachment Test
Learn more about the Retinal Detachment Test and how it can help prevent permanent blindness.
Use Template
Retinal Detachment Test Template
Commonly asked questions
This is most typically conducted by an eye doctor following symptoms of vision changes.
These tests are usually recommended upon referral, or conducted by your eye doctor following any changes in vision. This includes any obstructions to vision, seeing dots or squiggly lines, or blurred sight.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











