ROM testing involves assessing the extent of joint movement to determine the flexibility and mobility of a specific joint.
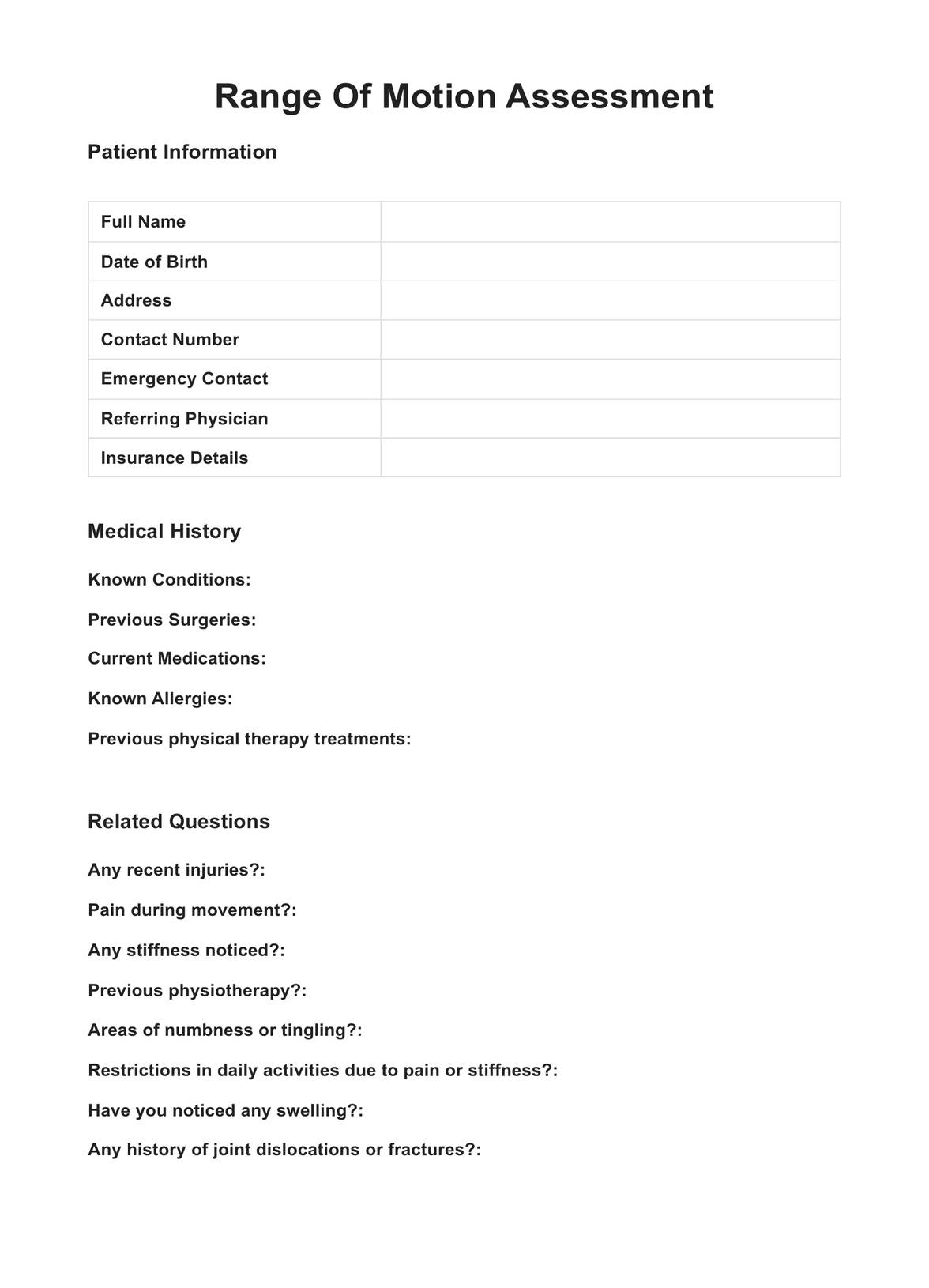
Range Of Motion Assessment
Dive into the revolution of assisted living care with Carepatron. Discover the comprehensive Range Of Motion Assessment guide, and enhance your care professionalism today.
Use Template
Range Of Motion Assessment Template
Commonly asked questions
ROM is measured using a goniometer or similar device, which quantifies the angle of joint movement during specific motions.
Limited ROM suggests restricted joint mobility, which may indicate underlying issues such as stiffness, muscle tightness, or joint injury.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











