Monitoring vital signs post-surgery is crucial as it helps detect any early signs of complications. Changes in blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation can indicate bleeding, shock, infections, or adverse reactions to anesthesia.
Post-Op Nursing Assessment
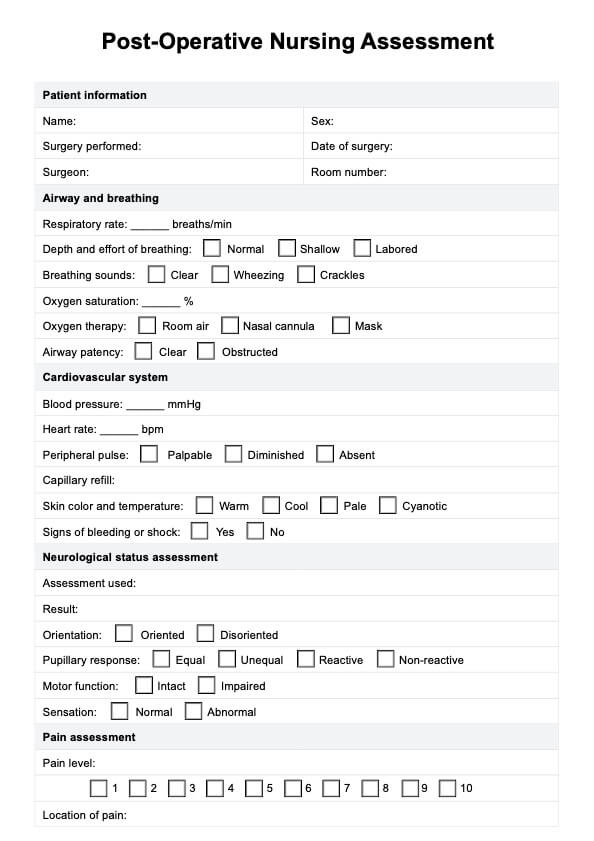
Optimize recovery through this efficient post-operative nursing assessment for comprehensive patient care and better health outcomes.
Post-Op Nursing Assessment Template
Commonly asked questions
Signs of infection at a surgical site include redness, swelling, increased warmth, drainage (particularly if it's purulent or foul-smelling), and increased pain or tenderness. Regular surgical site assessment is critical to identify and address these signs promptly.
Adequate pain relief and management after a major surgery is vital for various reasons. It helps improve patient comfort, promotes early mobility, facilitates effective breathing, and aids overall recovery. Uncontrolled pain can hinder movement, increase the risk of complications such as blood clots or pneumonia, and delay the healing process of surgical patients.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











