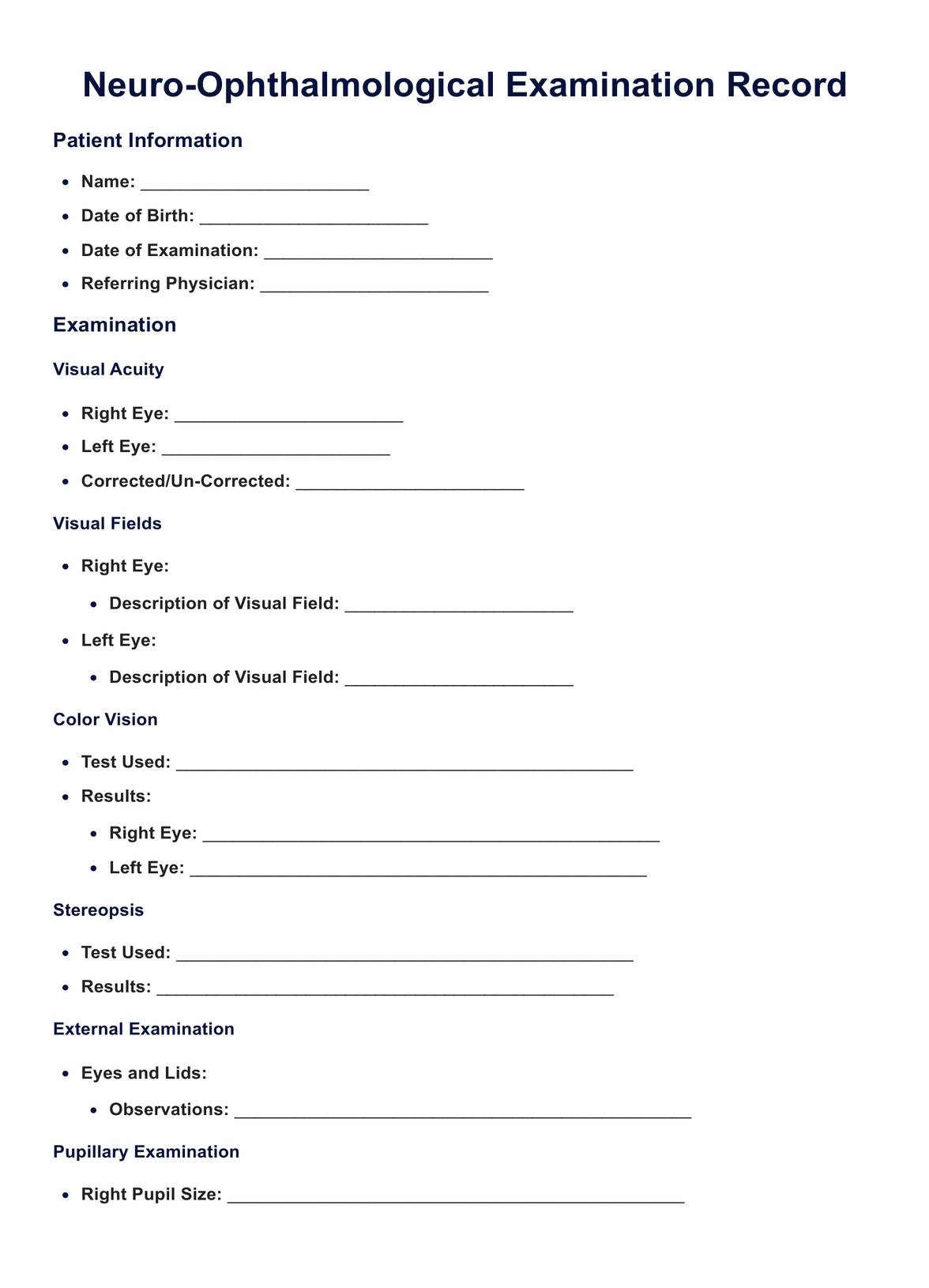
A neuro-ophthalmological assessment for visual loss includes evaluating the best corrected visual acuity for distance and central vision. Tests like fundus examination and optical coherence tomography (OCT) assess the health of the optic nerves and macula. The assessment may include pupil testing, confrontation visual fields, and a detailed review of any refractive error. The neuro-ophthalmologist aims to diagnose macular degeneration, optic neuritis, or central serous retinopathy.