A neuromuscular transmission defect is an impaired communication between nerves and muscles, a Myasthenia Gravis (MG) hallmark. Testing helps identify and assess these defects.
Myasthenia Gravis (MG) Test
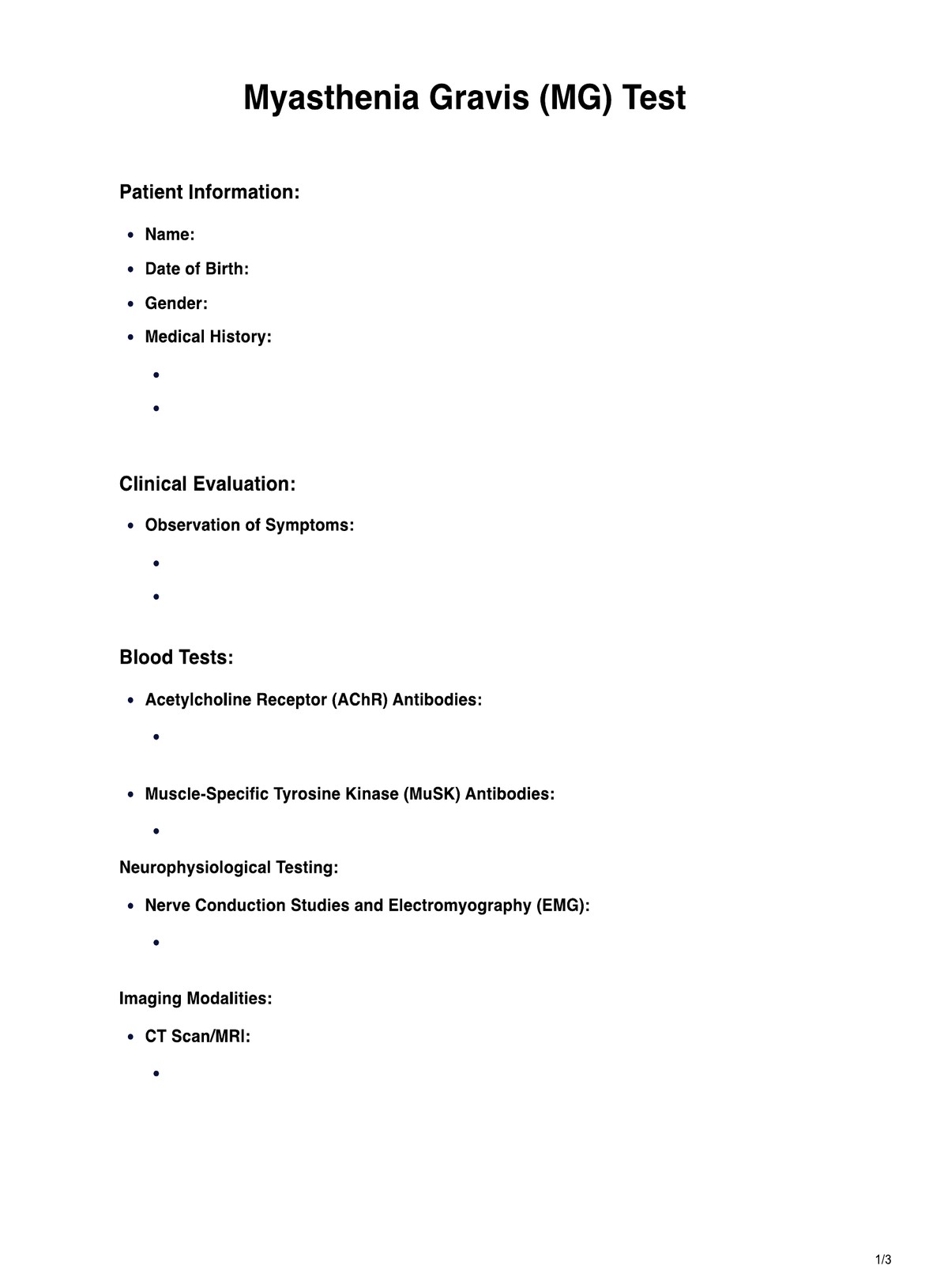
Accurate Myasthenia Gravis (MG) Test for precise diagnosis and treatment planning. Trust our healthcare expertise for reliable results and personalized care.
Use Template
Myasthenia Gravis (MG) Test Template
Commonly asked questions
MG can affect muscles responsible for breathing and blood pressure regulation. Testing helps evaluate respiratory function and ensures proper management to prevent complications.
MG is complex, and various tests, including blood tests, neuroimaging, and electrodiagnostic tests, are essential for a comprehensive understanding of the disease.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











