The Morse Fall Scale (MFS) is commonly used in hospitals, long-term care facilities, and other healthcare settings to assess fall risk among patients. It is particularly effective for hospitalized and elderly patients. After scoring, healthcare providers can develop personalized fall prevention plans based on the identified risk factors.
Morse Fall Scale
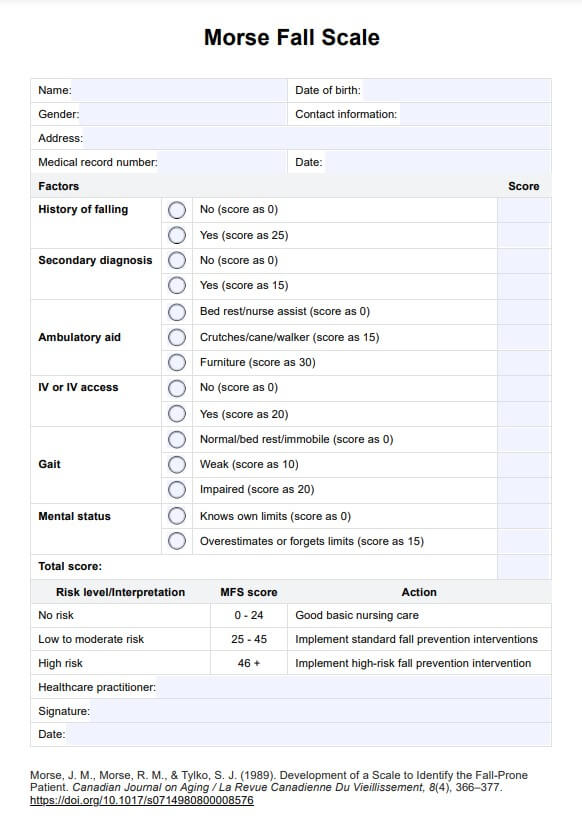
Use the Morse Fall Scale (MFS), a fall risk tool, to assess the fall risk of patients to help you determine appropriate interventions and safety precautions.
Morse Fall Scale Template
Commonly asked questions
No. It's meant to assess patients in inpatient/hospital settings. It's best to use other fall risk and balance assessment tools like the Berg Balance Scale and the Tinetti Balance and Gait Test to assess patients and create interventions for them in environments outside clinical settings.
Besides injuries and death, it can significantly impair the patient's mobility and balance, which affects their ability to move and perform activities of daily living independently.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











