A Medicare cheat sheet is a concise reference guide that outlines essential documentation requirements and guidelines for Medicare claims. It simplifies complex regulations, making it easier for healthcare providers to ensure compliance and accuracy in their documentation.
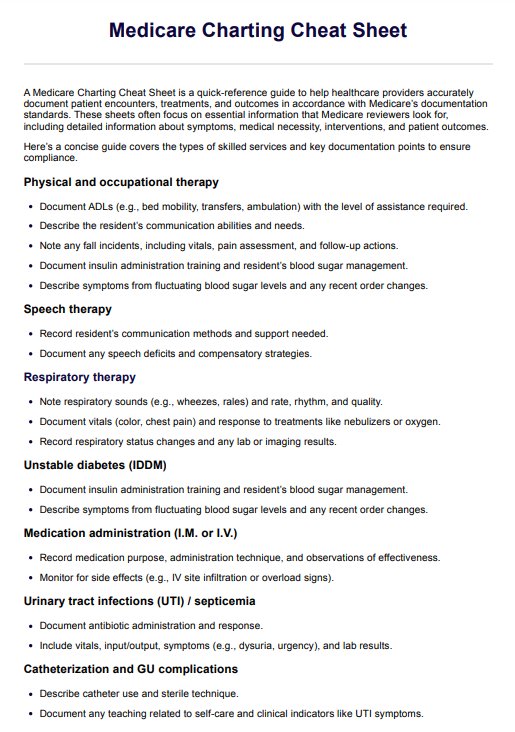
Medicare Charting Cheat Sheet
Streamline your documentation with our Medicare Charting Cheat Sheet, enhancing accuracy, compliance, and efficiency for healthcare providers.
Medicare Charting Cheat Sheet Template
Commonly asked questions
A Medicare cheat sheet can benefit healthcare practitioners in various settings, including hospitals, nursing homes, and private practices. It is a valuable resource for physicians, nurses, billing specialists, and administrative staff involved in the documentation and billing processes.
By providing clear and organized information, a Medicare cheat sheet helps practitioners quickly find necessary guidelines for documentation. This improved efficiency reduces the likelihood of errors in claims submissions and ensures that all required elements are included, facilitating smoother billing processes.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











