Dermatomyositis is diagnosed through clinical evaluation, muscle and skin biopsies, imaging studies, and laboratory tests.
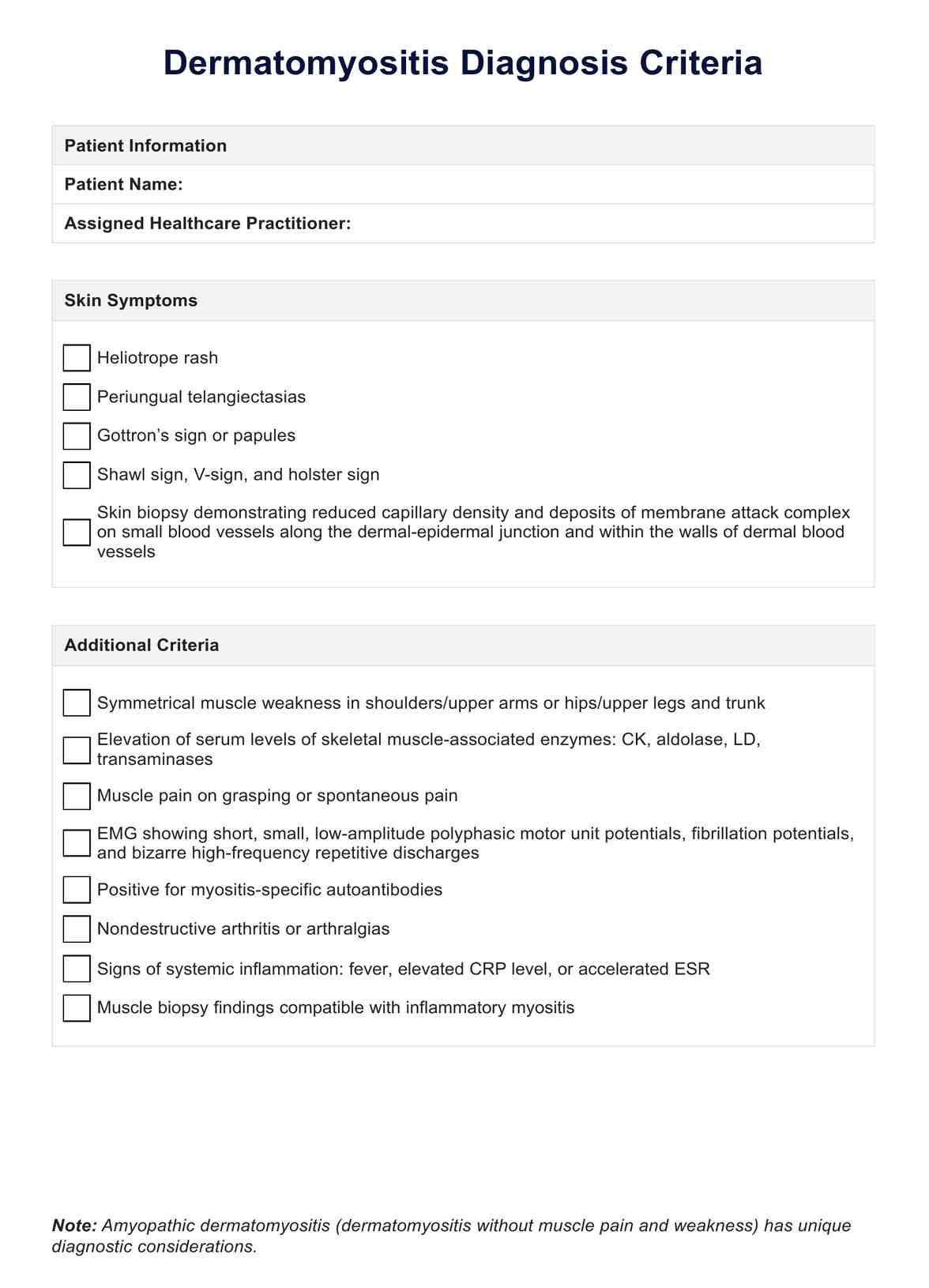
Dermatomyositis Diagnosis Criteria
Learn about the diagnostic criteria for dermatomyositis and see an example with Carepatron's free PDF download. Get the information you need to understand this condition.
Use Template
Dermatomyositis Diagnosis Criteria Template
Commonly asked questions
A muscle biopsy is the gold standard for diagnosing dermatomyositis, which can reveal characteristic histopathological findings such as muscle inflammation and necrosis.
Common abnormal laboratory findings in dermatomyositis include elevated levels of muscle enzymes such as creatine kinase (CK) and aldolase and abnormal electromyography (EMG) results.
EHR and practice management software
Get started for free
*No credit card required
Free
$0/usd
Unlimited clients
Telehealth
1GB of storage
Client portal text
Automated billing and online payments











